TF-6: Accelerating SDGs: Exploring New Pathways to the 2030 Agenda
This policy brief emphasises the complexity and urgency of sustaining malaria elimination in fragile, conflict-affected, and disaster-prone areas. It addresses how humanitarian crises disrupt malaria prevention and treatment interventions, exacerbating the health crisis. It urges the G20, which represents the world’s major economies, to lead efforts in tackling malaria by leveraging its economic and political influence. The recommendations include increasing funding, particularly through innovative private-sector involvement, and strengthening cross-sector collaboration between governments, international organisations, and businesses. Tailored interventions that address social determinants such as poverty and access to healthcare, and the integration of malaria control into disaster management strategies are also highlighted. The brief also promotes utilising existing platforms and case studies to facilitate knowledge sharing and build resilience. In essence, it calls for a cohesive, adaptive, and well-resourced approach involving various stakeholders to build resilient health systems for malaria elimination in crisis-laden environments.
1. The Challenge
Malaria-endemic countries often face health and humanitarian crises unrelated to the global crises such as the COVID-19 pandemic. In 2021, an estimated 268 million people were dealing with humanitarian crises, compared to 301 million in 2020.[1] In the Democratic Republic of the Congo, for example, the malaria prevalence in conflict-affected regions reached an alarming 59 percent in 2020. The ongoing civil war in Sudan is a tragic illustration of how such conflicts can have a devastating effect on healthcare systems. Since mid-April, the conflict has caused widespread disruptions, including the closure of over 70 percent of hospitals, the bombing of numerous facilities, and the routine necessity of forced evacuations.[2]
Figure 1: People in humanitarian need in malaria-endemic countries (as of December 2021).
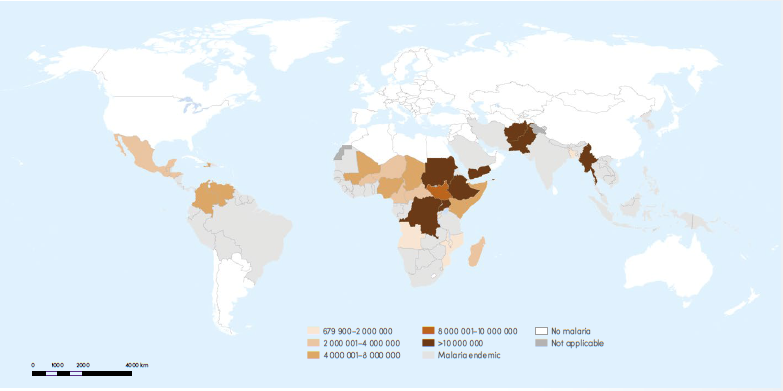
Source: WHO[3]
Service delivery of malaria prevention and treatment interventions
Malaria elimination programmes are mostly intervention-based, focusing on delivering services to the last mile of vulnerable populations. These include early diagnosis and case management, vector control interventions such as Indoor Residual Sprays and Long-Lasting Insecticidal Nets, and Social and Behavioural Change Communication interventions.
In the event of civil unrest or natural disasters, these interventions are disrupted due to unsafe working conditions including risk of life, compromised health and civic infrastructure, and deprioritisation of non-essential services. Rescue operations, resuming stability in governance, ensuring food, shelter, and community safety become the primary focus areas. Quicker recovery of malaria elimination services may be seen in disaster situations. However, in case of civil unrest, the path to recovery is often stagnated.
In the northern governorate of Sa’ada in Yemen, the ongoing conflict between the government and Shia-Al Houthi rebels since 2004, has resulted in the disruption of health care services. In 2020, the problem was compounded by heavy rainfalls that escalated the incidence of dengue cases[a] following the disruption of clean water supplies and water stagnation in various damaged civil structures.[4],[5]
Disaster management policies focus on ‘stop-gap’ measures
In malaria elimination, disaster policies focusing solely on stop-gap measures rather than inclusive responses can jeopardise progress. Ethically, in the immediate aftermath of a disaster rehabilitation efforts need to be prioritised, but a lack of planning can often undermine health systems and prevent malaria control efforts.
For instance, during Sierra Leone’s Ebola outbreak in 2015, the attention was mainly on the virus, neglecting malaria entirely. Consequently, malaria cases and fatalities rose substantially due to disrupted prevention and reduced healthcare access. The country witnessed a 50 percent increase in malaria cases in early 2015 compared to the previous year.[6]
Similarly, after the earthquake in Haiti in 2010, the devastation to healthcare infrastructure hampered malaria services. Poor coordination between international aid agencies and the Haitian government led to delays in medical supplies and subpar sanitation in displacement camps[7], resulting in about 1.5 times increase in malaria cases in 2010 compared to 2009.[b],[8]
2. The G20’s Role
The G20 is a forum composed of the world’s largest economies, representing around 80 percent of the global GDP. Naturally, it has the potential to play a significant role in addressing the policy challenges identified in sustaining malaria elimination progress in fragile, conflict-affected, and disaster-prone areas.
This year, the Health Working Group of the G20 Sherpa Track acknowledged that pandemic prevention, preparedness, and response require diverse, multi-sectoral, and multi-agency coordinated efforts. There is an emphasis on the need to strengthen and empower communities to become resilient against future health emergencies.[9] The group recognises that COVID-19 unearthed many weaknesses in health systems worldwide, but it also acknowledges that the pandemic provided countries with necessary opportunities to build more resilient health systems.
It should be noted that fragile, conflict-affected, and disaster-prone settings do not only affect the human health but also have a tremendous impact on environmental and animal health. Taking this into consideration, the G20, under India’s presidency, has elevated ‘One Health’ as a core element of discussion in multi-sectoral working groups and tracks related to health, environment, urban planning, agriculture etc.
The Disaster Risk Reduction Working Group (DRRWG) under the Sherpa Track also provides the perfect platform to discuss malaria elimination in disaster-affected settings. This group was founded in the aftermath of the Nargis Cyclone in Myanmar in 2008. Currently, it consists of over 53 agencies including the UN, international NGOs, local NGOs, and professional organisations working towards DRR.[10]
3. Recommendation to the G20
To address the challenges and reduce the impact of malaria, the following recommendations can be considered by both (a) malaria-free countries to prevent a re-introduction of disease in the aftermath of a disaster, and (b) malaria-endemic countries to ensure acceleration of gains towards malaria elimination.
Increase funding for malaria elimination efforts in fragile and conflict-affected states
Global data reveals that the estimated share of the extreme poor living in fragile and conflict-affected states (FCAS) will rise from 17 percent to 60 percent by 2030.[11] This is a deeply concerning statistic. Fortunately, this has not gone unnoticed, and an increasing number of donors are stepping up to support the health situations in FCAS.[12] In addition to support from external donors, recipient countries should also have the capacity to optimally utilise this support, as ‘aid coordination’ is a significant factor for the FCAS.[13]
To sustain progress in malaria elimination in fragile, conflict-affected, and disaster-prone states the G20 can use its collective economic and political influence to promote increased funding and resources for malaria control programmes. The G20 member countries should lead by example by addressing social inequities that increase vulnerability to malaria. This includes improving access to health services and prevention tools for marginalised and disadvantaged populations, including refugees, internally displaced persons, and other vulnerable groups. Some specific examples include:
Funding mechanisms: The G20 can ensure that progress towards malaria elimination is sustainable and benefits all populations. This includes supporting the Global Fund, which works to accelerate the end of HIV, tuberculosis, and malaria. The Global Fund has invested over US$19 billion in malaria programs since its inception in 2002, supporting interventions such as distributing insecticide-treated bed nets, indoor residual spraying, and diagnosing and treating malaria cases.[14] During the Indonesian G20 presidency, the Pandemic Fund was launched which can provide financial assistance and incentives to countries for prioritising pandemic prevention, preparedness, and response.[15]
Private sector: The G20 secretariat can encourage member countries to provide financial incentives to the private sector through taxe breaks and more so that such funding can be invested in disease elimination efforts during a crisis. This can also link back to supporting public-private partnerships that promote developing and distributing innovative tools for malaria control and elimination. A recent example is the Pandemic Emergency Financing Facility (PEF) established by the World Bank to provide financial support to countries during pandemics. The PEF includes a private sector window that incentivises private investment in pandemic preparedness and response. The initiative also supports developing and distributing innovative disease control and elimination tools.[16]
A key example of a malaria-specific initiative is the Medicines for Malaria Venture, a public-private partnership aiming to develop and deliver effective and affordable antimalarial drugs using Product Development Partnerships (PDPs). These PDPs address the lack of commercial incentive to develop tools to combat diseases in the developing world. PDPs use donor funds to entice the pharmaceutical industry and research institutions to conduct R&D for diseases they would otherwise be unable or unwilling to pursue independently.[17]
Another example of a private donor providing coordination support during a humanitarian crisis is the case of the Paul G. Allen Family Foundation during the Ebola outbreak in West Africa between 2014 and2016. The Paul G. Allen Family Foundation, a private philanthropic organisation, provided funding and coordination support to various organisations involved in the Ebola response effort, including the US Center for Disease Control and Prevention, the World Health Organisation (WHO), and Médecins Sans Frontières.[18]
Strengthen collaboration and partnerships between governments, international organisations, and the private sector
Fragile, conflict-affected, and disaster-prone situations are unpredictable and are usually localised within a country. Utilising first-hand experience and external aid, countries develop specialised skills and capacities. It’s crucial to bolster these through collaboration among governments, international organisations, and businesses. A systematic framework outlining mutual goals, responsibilities, resources, and accountability is necessary for coordinated and sustainable partnerships. Here are the most impactful thematic areas for collaboration:
Tailoring malaria response in fragile, conflict-affected, and disaster-prone states: The Differential Vulnerability Framework draws attention to the fact that different populations are vulnerable to public health threats differently, based on social, economic, and environmental factors.[19]Understanding and strategically addressing these social determinants is imperative in the context of malaria.
Poverty is a key factor, as those living in poverty often lack resources for prevention and treatment of malaria. Moreover, impoverished areas might have substandard housing and sanitation facilities, increasing the risk of mosquito breeding. Living conditions are intrinsically connected to malaria transmission. Crowded or poorly built housing, common in impoverished areas, can increase mosquito exposure. Additionally, in conflict or disaster zones, people might end up in temporary shelters that don’t offer sufficient protection.
Environmental factors are also vital. For instance, areas with stagnant water are potential breeding grounds for mosquitoes. Implementing strategies for environmental management, such as proper waste management and draining of stagnant waters, can effectively control the spread of malaria.
In the same vein, access to healthcare is central to preventing and eliminating mosquito-borne diseases. In fragile regions, the health infrastructure may be weakened or non-existent. Strengthening access involves not just improving the availability of medicines but also ensuring there are enough capable healthcare providers.
It is also essential to prioritise proactive prevention and preparedness measures, such as strengthening early warning systems, disaster risk reduction strategies, and integrating malaria control efforts into overall disaster management plans. This can involve mapping and monitoring mosquito breeding sites, engaging communities in vector control activities, and strengthening surveillance systems to enable early detection of malaria cases.
At the core of these considerations is the urgent need to develop gender-sensitive programs. We must acknowledge that gender roles and norms can limit womens’ and other vulnerable groups’ access to healthcare services. This can only be addressed by developing interventions that address these socio-economic barriers. Additionally, human rights must be central to malaria elimination efforts. Ensuring marginalised populations, including refugees, internally displaced persons, and those affected by conflicts, have equitable access to health services and are not discriminated against, is key to the success of any malaria elimination effort.
Existing mechanisms should be adapted to include malaria interventions as part of the overall humanitarian response. For instance, the MENTOR initiative, which trains and supports Community Health Workers, provides primary healthcare for displaced communities and is active in several countries.[20]
Scaling up innovative approaches to build capacity and improve collaboration: To address malaria in fragile settings, ensuring continuous capacity for delivering aid, including malaria interventions, is vital. The G20 should prioritise capacity-building and knowledge-sharing initiatives, demonstrate successful interventions, and leverage the G20 platform for dissemination of crucial information. Coordination among partners can be improved through joint task forces, resource pooling, and centralised data sharing.
The Public Health Emergency Preparedness framework offers a comprehensive approach focusing on building infrastructure, enhancing surveillance systems, improving communication, and promoting collaboration across different sectors.[21] The G20 member countries can also bolster existing platforms, such as the WHO’s Health Cluster Dashboard, and build cross-sectoral bridges between relevant UN offices.[22]
Furthermore, integrating succinct monitoring and evaluation (M&E) is crucial for assessing program effectiveness. M&E involves routine data collection and analysis to gauge progress and outcomes. This enables: a) optimisation through the identification of successful interventions, b) increased accountability and transparency, and c) evidence-based decision-making and policy adaptation.
Efficient M&E strategies should encompass data collection via surveys, health information systems, and surveillance. Using digital health technologies, such as mobile applications, can enhance M&E systems’ efficiency. Incorporating M&E ensures programs remain responsive to the needs of populations in A settings and contributes to sustainable malaria elimination.
Coordinating mechanisms for partnerships: A coordinating mechanism for partnerships would work closely with affected countries and communities to ensure that malaria elimination efforts are context-specific and respond to these populations’ unique needs and challenges. The G20 platform should also support the development of partnerships with non-governmental organisations, academic institutions, and the private sector to leverage expertise, resources, and innovation towards malaria elimination efforts.
The strength of public-private partnerships in malaria elimination programmes has been demonstrated in FCAS countries such as Sri Lanka[23] and the challenging geographies of India.[24] However, these initiatives are often referred to as ‘islands of excellence’ and the national governments have not mainstreamed the public-private-partnership mode of operation. The G20 should leverage their authority to highlight the benefits of collaborations between private organisations with defined accountability and government-owned disease elimination initiatives.
One of the ways to achieve cohesiveness in the proposed partnerships is to utilise the ‘Health in All Policies (HiAP) framework’, which is a comprehensive approach that recognises the interconnectedness of various sectors, policies, and health outcomes. It emphasises the importance of collaboration and coordination across different sectors and disciplines to address complex health challenges.[25] The HiAP framework can provide a useful approach to address the social determinants of health that underlie malaria transmission and address the complex challenges faced by health systems in fragile and conflict-affected regions. For example, improving water and sanitation infrastructure can help reduce mosquito breeding sites and the risk of malaria transmission. Similarly, promoting agricultural practices that reduce standing water, where mosquitoes breed, can help limit the spread of malaria.
Case Study: Malaria Elimination in Sri Lanka
Context: The Sri Lankan civil war lasted from 1983 to 2009. Despite the related impacts and setbacks, the country eliminated malaria in 2016.
Challenges: Conflict restricted access to malaria-affected populations and hindered the distribution of insecticide-treated nets and anti-malarial drugs.
Initiatives and lessons learned: The National Malaria Control Program worked closely with the International Red Cross and several NGOs to deliver services across conflict lines. Mobile malaria clinics were used to reach displaced populations. The key lesson learnt is that flexibility and collaboration with humanitarian agencies can facilitate malaria control during periods of conflict.[26]
Attribution: Harsh Rajvanshi, Viola D’souza, and Sanjay M. Pattanshetty, “Sustaining Progress on Malaria Elimination in Fragile, Conflict-Affected, and Disaster-Prone Areas,” T20 Policy Brief, July 2023.
Endnotes
[a] In 2019, Yemen reported 192 deaths caused due to dengue. In the first two weeks of January 2020, 78 deaths were reported 78 deaths, which was primarily attributed to heavy rainfalls amidst a fragile health system.
[b] The Ministère de la Santé Publique et de la Population reported 28,993 malaria cases in 2009 and 36,106 in 2010. The WHO reported 49,535 (2009) and 84,153 (2010) malaria cases.
[1] World Health Organisation, World Malaria Report, 2022, Geneva,WHO, 2022.
[2] Harriet Pasquale et al., “Malaria Control in South Sudan, 2006–2013: Strategies, Progress and Challenges” Malaria Journal 12, no. 1 (October 27, 2013).
[3] WHO, World Malaria Report, 2022, 9
[4] May Meleigy, “Yemen Conflict Takes Its Toll on Civilians,” The Lancet 375, no. 9711 (January 1, 2010): 269–70.
[5] UNICEF, Yemen Humanitarian Situation Report 2020, January 2020, UNICEF.
[6] Alyssa S. Parpia et al., “Effects of Response to 2014–2015 Ebola Outbreak on Deaths from Malaria, HIV/AIDS, and Tuberculosis, West Africa,” Emerging Infectious Diseases 22, no. 3 (March 1, 2016): 433–41.
[7] United Nations, Report of United Nations in Haiti 2010: Situation, Challenges, and Outlook, Haiti, 2011, UN.
[8] Jean Ricardo Jules et al., “Malaria in Haiti: A Descriptive Study on Spatial and Temporal Profile from 2009 to 2018,” Revista Da Sociedade Brasileira De Medicina Tropical 55 (January 1, 2022).
[9] Ministry of Health and Family Welfare, Government of India.
[10] “Disaster Risk Reduction Working Group (DRRWG), Devex.
[11] OECD, States of Fragility 2022, Paris, OECD, 2022.
[12] Aniek Woodward et al., “Health Systems Research in Fragile and Conflict-Affected States: A Research Agenda-Setting Exercise,” Health Research Policy and Systems 14, no. 1 (July 21, 2016).
[13] Maria Paola Bertone et al., “Health Financing in Fragile and Conflict-Affected Settings: What Do We Know, Seven Years On?,” Social Science & Medicine 232 (July 1, 2019): 209–19.
[14] World Bank Group, G20 Hosts Official Launch of The Pandemic Fund, World Bank, November 28, 2022.
[15] “Financial Intermediary Fund for Pandemic Prevention, Preparedness, and Response – PPR FIF,” World Bank, 2023.
[16] World Bank Group, “Pandemic Emergency Financing Facility,” World Bank, June 3, 2022.
[17] “About Us,” Medicines for Malaria Venture, Accessed June 20, 2023.
[18] “Paul G Allen back two new initiatives in the fight against the Ebola virus”, September 15, 2014, UNICEF.
[19] Subhakanta Mohapatra, “Assessing differential health vulnerability of the slums in Chandigarh, India.” Internationales Asienforum 43, no. 1-2 (2012): 81-98.
[20] Kathryn Johnson, “Primary Healthcare in the Community,” The MENTOR Initiative, March 8, 2023.
[21] Yasmin Khan et al., “Public Health Emergency Preparedness: A Framework to Promote Resilience,” BMC Public Health 18, no. 1 (December 1, 2018).
[22] “Health Cluster Countries and Regions.” World Health Organization. Accessed June 20, 2023.
[23] Sumadhya Deepika Fernando et al., “Use of a Public-Private Partnership in Malaria Elimination Efforts in Sri Lanka; a Case Study,” BMC Health Services Research 18, no. 1 (March 23, 2018).
[24] Harsh Rajvanshi et al., “Learnings from Two Independent Malaria Elimination Demonstration Projects in India,” Transactions of the Royal Society of Tropical Medicine and Hygiene 115, no. 11 (September 25, 2021): 1229–33.
[25] Enhanced Wellbeing, “Health in All Policies: Helsinki Statement. Framework for Country Action,” World Health Organisation, April 23, 2014.
[26] Rabindra R Abeyasinghe et al., “Malaria Control and Elimination in Sri Lanka: Documenting Progress and Success Factors in a Conflict Setting,” PLOS ONE 7, no. 8 (August 29, 2012).





