Task Force 2: Our Common Digital Future: Affordable, Accessible and Inclusive Digital Public Infrastructure
Digital public infrastructure (DPI) for health has significant economic, cross-sectoral, and population health benefits. For DPI for health, the World Health Organization (WHO) recommends digital enterprise architecture across a nation’s health sector and provides a categorisation of digital health interventions (DHIs). Given that G20 countries invest significantly in the health of their own populations and contribute the majority of WHO’s funding, they can take the lead by demonstrating the value of DPI for health investments in their own countries and by encouraging WHO to further strengthen its definitions of DPI for health. In partnership with G20 countries and low- and middle-income countries (LMICs), WHO should further develop DPI by providing guidance on vendor-agnostic requirements and DHIs, and set standards for a nation’s cloud-based enterprise architecture (EA) and DHI. This guidance should include vendor-agnostic workflows, minimum datasets, relevant metadata, standards for privacy, security, and interoperability, and other requirements.
1. The Challenge
1.1 Benefits and current status of DPI for health
DPI for health is critical for public health and achieving other SDGs. DPI refers to “population-scale digital systems and platforms supporting basic, society-wide functions.”[1] WHO defines ‘digital health enterprise’ as “the business processes, data, systems and technologies used to support the operations of the health system, including digital health applications, point-of-service software applications, other software, devices, hardware, standards, governance and underlying information infrastructure functioning in a purposeful and unified manner.”[2] While there is no global consensus on the definition of DPI for health, WHO’s formulation is interchangeable with DPI for health. Some components of the digital health enterprise may be run by the private sector, but this should be shaped as part of a country’s health system, and the public sector should have a key role in developing and regulating national digital health enterprises. (Section 2.2 provides details on digital health enterprise.)
DPI for health is critical for promoting individual, public, and population health, and as a component of broader DPI, for promoting the Sustainable Development Goals (SDGs) because of health’s intersection with other sectors, such as education (e.g. health literacy), finance (e.g. financial services for health), agriculture (e.g. nutrition), and environment (e.g. environmental risks to health).
Benefits to patients and population health
A systematic review identified studies, including randomised controlled trials, that demonstrate beneficial outcomes in outpatient, inpatient, emergency, and community settings from health information exchange (HIE).[3] These include fewer repeat interventions or imaging, improved detection of medication discrepancies, and decreased testing per patient.
A subsequent review examined the global evidence of HIE. It found studies showing improvements in healthcare quality and utilisation with reductions in hospital readmissions, hospital-acquired infections, or duplicate testing and prescriptions. HIE can also improve care transitions, enable shared decision-making, and improve patient satisfaction.[4] DPI for health is critical to information exchange between organisations, especially government agencies. Unfortunately, most research on this topic is from high-income countries; there is a need for further research in LMICs.
DPI for health can also improve access to care, such as national eligibility determinations being facilitated via the integration of eligibility and enrolment systems.[5],[6]
Economic benefits
The most comprehensive economic impact assessment for investing in DPI for health comes from the European Commission (EC)’s proposed European Health Data Space (EHDS) regulation. The EU estimates that primary uses of health data over ten years could be valued between 5.57 billion and 5.63 billion euros, and from secondary uses, 5.4 billion euros.[a],[7],[8] While the benefits and costs would vary across geographies, the EU’s impact assessment illustrates the possible benefits. An analysis from the UK found that consolidating NHS data into longitudinal data would bring about £9.6 billion per year in savings.[9]
Despite progress in digital health, many countries, including G20 countries and LMICs, have limitations in their DPI for health.
While every geographical area is at a different stage of maturity in its DPI for health, many face continued challenges. The following examples from select countries and regions highlight the problems and challenges.
United States
The COVID-19 pandemic highlighted the fragmentation of the US health data infrastructure and its effect on public health, particularly between healthcare and public health organisations. For example, state public health agencies and local health departments face barriers in bidirectional data reporting and exchange amongst themselves and with clinical providers.[10],[11] Moreover, when asked about the barriers, US healthcare providers cited that the principal barrier was that agencies could not receive data electronically.[12] In addition, DPI for health at the state, tribal, local, and territorial (STLT) level is underfunded, requiring between $8 billion and $37 billion to fund STLT public health data systems over the next 5–10 years.[13],[14]
Europe
In 2022, the European Commission (EC) published its proposed regulation for establishing the European Health Data Space (EHDS). Its DPI aims to support the use of health data for better healthcare delivery and research, enable the safe and secure exchange of health data, and provide individual access to and ownership of health data.[15] In its reports to the European Parliament, the Commission notes that not all member states have exchange systems for electronic health records (EHR) data and that their systems exhibit significant interoperability challenges. For instance, electronic summaries and prescriptions of patients are available in two-thirds of member countries, but only a few can be sent and received across borders. In addition, while MyHealth@EU serves as a cross-border DPI for health, only 10 member countries support cross-border access to these electronic summaries and prescriptions. Other data, such as imaging and laboratory results, are yet to be exchanged through MyHealth@EU.[16]
United Kingdom
The current digital infrastructure in the UK relies on multiple segregated systems that are costly duplication of records and fail to provide the full health history of an individual, thus affecting patient care. Data sharing for analytics and decision-making has thus far relied on pseudonymisation—now acknowledged as a weak security practice.[17] Since the review, the NHS published its plan for digital health and social care, where it intends to digitise and combine health and social care records as key foundational investments alongside using regulatory, standards and investment levers.[18] It also published a data strategy proposing the establishment of federated data platforms and trusted research environments through which health data can be securely accessed by authorised users who can then curate and analyse the data for decision-making and research.[19]
Africa
As of 2019, 34 African countries had developed digital health strategies, which focus on the nations’ digital health infrastructure, standards, and interoperability to improve the utilisation of digital health tools. However, only 12 have implemented their digital health strategies. While the use of digital health solutions has increased, most solutions are pilots rather than nationwide DPI for health, and the majority do not adhere to WHO-recommended implementation methodologies.[20]
Similarly, a scoping review on the use of DHIs in Sub-Saharan Africa for the strengthening of health systems found that half of the interventions used between 2011 and 2021 were not at an ‘established’ stage of development.[21] These findings indicate the need to target investments towards holistic, health enterprise-wide solutions.
Asia
Digital health infrastructure and strategies vary drastically across Asia and are often challenged by the diverse geography of the region and the ever-growing digital divide among the population.[22] For instance, a scoping review of five Asian countries concluded that although digital health policies existed in all, they often lacked supporting legislations and regulations to govern standards and interoperability.[23] Another study, this time focused on Bhutan—a country with a fragmented digital health system—found that data sharing was highly inefficient, limiting the means to conduct analytics and care coordination.[24]
Latin America
Latin America currently experiences a large digital divide, and there is currently no standardisation and interoperability within existing health systems. As a result, there has been mixed adoption of digital infrastructure, causing development in digital health to stagnate. For instance, a report found that only 11 countries have regulations to validate EHRs as of 2021, and only 14 (out of the 26 countries studied) have a digital health strategy.[25] Only 27 percent of these countries have regulations for the transition from paper-based to digital records, and less than 50 percent have acknowledged and included interoperability standards in their national regulations for EHRs.[26] The dearth of essential policies for digital health in the region has resulted in fragmented systems where healthcare workers are unable to access complete and accurate health records.[27]
1.2 WHO currently recommends EA to develop a digital health enterprise and DHIs for countries. WHO should provide vendor-agnostic requirements and set standards for cloud-based national digital health EA and DHIs.
Because digital health systems are fragmented in many geographies, the best practices and normative guidance were reviewed in an attempt to identify best practices to make them more integrated. A literature review of publications produced or referenced by WHO was undertaken to understand the scope for WHO to strengthen normative guidance to countries on DPI for health.
WHO recommends that nations adopt digital EA across the health sector, and provides a specific list of DHIs. WHO recommends seven steps for planning and implementing a digital health enterprise: 1) assessing the current state and enabling environment; 2) establishing a shared understanding and strategic planning; 3) defining the future state; 4) planning the enterprise architecture; 5) determining health content requirements; 6) monitoring and evaluating digital health implementations and fostering data use; and 7) implementing, maintaining, and scaling.[28] These recommendations and guidance are important contributions to normative guidance on DPI for health.
WHO can further develop its guidance on DPI for health in three ways:
- WHO’s list of DHIs can make public health administration end-users and use cases more explicit (such as planning national immunisation campaigns).
- WHO can support countries by providing guidance on vendor-agnostic requirements and set standards for a nation’s cloud-based EA and DHIs. This guidance should include vendor-agnostic workflows, minimum datasets, relevant metadata, standards for privacy, security, and interoperability.
- WHO can establish a standing expert committee to regularly review and update this guidance on vendor-agnostic requirements.
WHO normative guidance on EA
WHO recommends implementing ‘exchanged’ EA and provides multiple conceptual schematics for what this means (Figure 1).[29] WHO also describes key components of a nation’s digital health EA, including, business domain services, registry services, data sources, data services, and point-of-service applications.
Figure 1. WHO Schematic for Exchanged EA[30]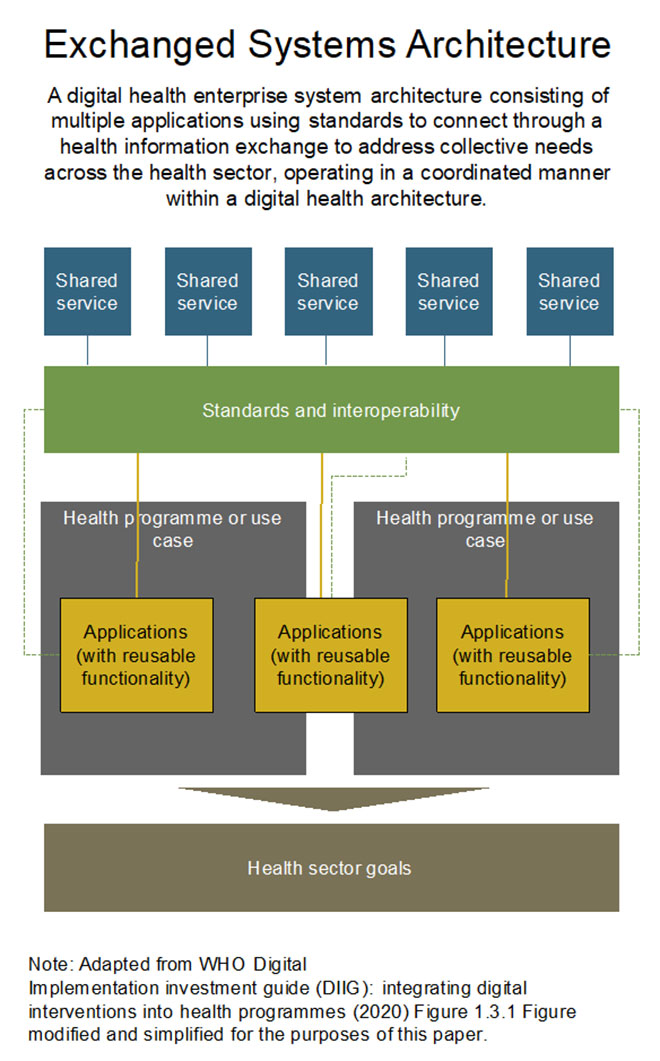
WHO normative guidance on DHIs
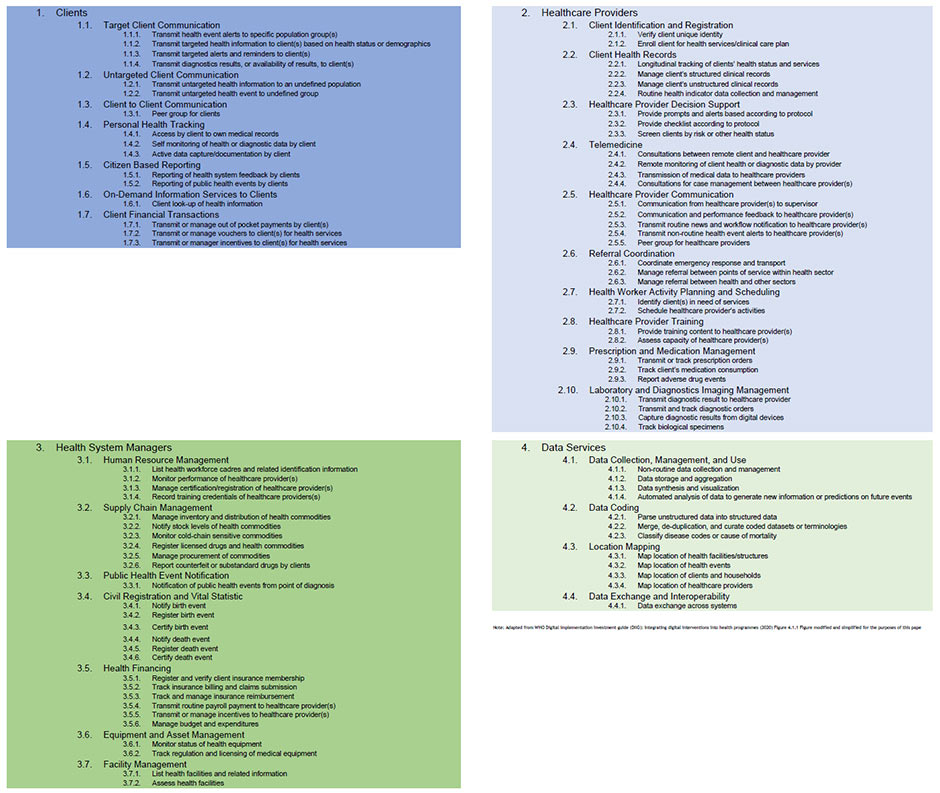
WHO classifies DHIs into groups based on the targeted primary user (Figure 2). These DHIs provide a useful starting point for countries. However, they do not explicitly include public health end-users, and use cases for public health administration or population health management that cover a country (or sub-national geography spanning multiple clinical providers), such as national immunisation campaigns.
Figure 2. WHO’s Classification of DHIs [31]
WHO guidance on vendor-agnostic requirements and standards
WHO’s normative guidance on DPI for health does not include vendor-agnostic standards and functional requirements. Without normative guidance from WHO, investments in DPI for health will remain fragmented and lead to systems that face challenges with interoperability, data exchange, and other core functionalities. With the exception of three ‘digital adaptation kits’ (DAKs), which are specific to certain diseases health domain, WHO currently has limited normative guidance on functional requirements and standards for DPI for health.[32]
According to WHO, “There are currently no explicit international or national policies requiring the use of standards when developing digital health systems.”[33] WHO guidance documents inevitably draw a comparison to the standards set by the International Telecommunication Union (ITU), International Organization for Standardization (ISO), Health Level Seven (HL7), and other organisations. However, the range of standard-development organisations is broad, and each defines and validates various standards which may or may not be complementary, can be duplicative, and can exhibit problems on usability and scalability.[34]
Therefore, WHO can support countries by providing guidance on vendor-agnostic requirements and standards for a nation’s cloud-based EA and DHIs. This guidance should include vendor-agnostic workflows, minimum datasets, relevant metadata, standards for privacy, security, and interoperability, and other requirements.
While EA and DHI implementation will differ by country based on infrastructure maturity, WHO could still set normative standards and requirements. WHO can also prioritise these requirements as basic, intermediate, and advanced functionality.
For example, PATH developed a product vision document for its better immunisation data (BID) initiative[35] with functional and non-functional requirements for immunisation systems. WHO’s DAKs take a similar approach, but are for disease-specific interventions and workflows, rather than for broader health information systems.
By developing normative guidance on requirements for EA and DHIs, WHO would help ministries of health (MOH) better design their systems and select solutions from IT vendors. Governments and funders should then use WHO guidance to set minimum requirements for vendors as they procure and develop their nation’s DPI for health.
2. The G20’s Role
The G20 can provide global leadership for countries, including G20 members and LMICs, to encourage the adoption of standardised DPI for health. As a leading multilateral body helping set the global agenda, the G20 is well-positioned to advance DPI for health as a focus area for governments and other multilateral organisations. Given that G20 countries typically have some of the highest health spending per capita, they should have significant resources to strengthen their own DPI for health, thereby innovating and demonstrating the value of DPI for health to the broader global community. According to WHO, G20 countries account for greater than 50 percent of its member state financial contributions, and therefore have an opportunity to influence its direction in DPI for health.[36]
3. Recommendations to the G20
G20 can promote the adoption of standardised DPI for health to help achieve a range of SDGs and government priorities. The G20 should consider the following:
- Include DPI for health in the broader DPI agenda.
- Policy, investments, and other efforts focused on DPI and digital public goods (DPGs) should include health as a critical sector, and should highlight the linkages between DPI for health and DPI for other sectors, such as financial services, or sectors included in WHO’s ‘One Health’ initiative (e.g. environment, agriculture, and veterinary).
- Encourage and fund WHO to develop vendor-agnostic functional requirements and set standards for a nation’s cloud-based EA and DHIs.
- These standards and requirements would be for both EA and DHIs. They would provide MOHs and other government agencies with clear guidance on what to look for when procuring solutions from IT vendors (or when developing custom solutions). They would similarly provide guidance to IT vendors developing DPI and technology solutions.
- Procure health information systems consistent with these requirements.
- G20 countries can lead not only by encouraging the development of these requirements, but also by using them in their own procurements.
- Structure funding to LMICs so that digital health investments conform to this guidance.
- Funding for digital health is typically fragmented and often encourages point solutions rather than investments in broader EA and DPI for health. Donors should ensure that their funding to LMICs for investments in digital health promotes the adoption of broader DPI that can serve a range of health use cases.
- These approaches to funding can be built on existing approaches and principles, such as the Principles of Donor Alignment for Digital Health.[37]
Attribution: Gabriel Seidman et al., “Strengthening Digital Public Infrastructure for Health,” T20 Policy Brief, July 2023.
Endnotes
[a] ‘Primary uses’ – the use of protected health information (PHI) by an entity that produced or acquired these data in providing real time, direct care of an individual. ‘Secondary uses’ – non-direct care uses of PHI, including but not limited to analysis, research, quality and safety measurements, public health, payment, provider certification or accreditation.
[1] World Economic Forum, “The Right Way to Build Digital Public Infrastructure,” World Economic Forum, 2022.
[2] World Health Organization, “Digital Implementation Investment Guide (DIIG): Integrating Digital Interventions into Health Programmes,” 2020.
[3] Nir Menachemi et al, “The Benefits of Health Information Exchange: An Updated Systematic Review,” J Am Med Inform Assoc, 25:9, 2018.
[4] Willi L Tarver, Pallavi Jonnalagadda, and Saurabh Rahurkar, “Evidence Base for Health Information Exchange,” Health Information Exchange, 2023.
[5] Center on Budget and Policy Priorities, “State Innovations in Horizontal Integration,” 2015.
[6] Sherry Glied, Sara Collins, and Saunders Lin, “Did the ACA Lower Americans’ Financial Barriers to Health Care? A Review of Evidence to Determine Whether the Affordable Care Act Was Effective in Lowering Cost Barriers to Health Insurance Coverage and Health Care,” Health Affairs, 39:3, 2020.
[7] European Commission, “Impact Assessment on the European Health Data Space,” 2022.
[8] Charles Safran et al, “Toward a National Framework for the Secondary Use of Health Data: An American Medical Informatics Association White Paper,” Journal of the American Medical Informatics Association, 14:1, 2007.
[9] Ernst & Young, “Realising the Value of Health Care Data: A Framework for the Future,” 2019.
[10]Association of State and Territorial Health Officials, “Profile of State and Territorial Public Health,” 2017.
[11] National Association of County & City Health Officials, “National Profile of Local Health Departments,” 2020.
[12] AJ Holmgren, Nate C Apathy, and Julia Adler-Milstein, “Barriers to Hospital Electronic Public Health Reporting and Implications for the Covid-19 Pandemic: The Authors’ Reply”, J Am Med Inform Assoc, 27:11, 2020.
[13] Council of State and Territorial Epidemiologists, “Modernize Public Health Data: A Call to Congress,” 2022.
[14] Healthcare Information and Management Systems Society, “Public Health Information and Technology Infrastructure Modernization Funding Report,” 2022.
[15] European Commission, “European Health Data Space,” 2020.
[16] European Commission, “Communication from the Commission to the European Parliament and the Council – a European Health Data Space: Harnessing the Power of Health Data for People, Patients and Innovation,” 2022.
[17] Ben Goldacre, Jessica Morley, and Nicola Hamilton, “Better, Broader, Safer: Using Health Data for Research and Analysis”, The Goldacre Review: Department of Health and Social Care, 2022.
[18] Department of Health and Social Care, “A Plan for Digital Health and Social Care,” 2022.
[19] Department of Health and Social Care, “Data Saves Lives: Reshaping Health and Social Care with Data,” 2022.
[20] World Health Organization’s Regional Committee for Africa, Report of the Secretariat – “Framework for Implementing the Global Strategy on Digital Health in the Who African Region,” WHO, 2021.
[21] Humphrey C Karamagi et al, “eHealth or E-Chaos: The Use of Digital Health Interventions for Health Systems Strengthening in Sub-Saharan Africa over the Last 10 Years: A Scoping Review,” Journal of Global Health, 12, 2022.
[22] The Economist Group, “Realising the Value of Digital Health in Asia and the Pacific,” 2022.
[23] Hui Chi Yan et al, “Mapping National Information and Communication Technology Infrastructure to the Requirements of Potential Digital Health Interventions in Low-and Middle-Income Countries”, Journal of Global Health, 12:1, 2022.
[24] Mongal Singh Gurung et al, “Transforming Health Care through Bhutan’s Digital Health Strategy: Progress to Date,” WHO South-East Asia Journal of Public Health, 8:2, 2019.
[25] Inter-American Development Bank, “The Golden Opportunity of Digital Health for Latin America and the Caribbean,” 2022.
[26] Inter-American Development Bank, “Regulatory Frameworks for Digital Health in Latin America and the Caribbean. Electronic Health Records: Progresses and Next Steps,” 2020.
[27] Pan American Health Organization, and World Health Organization, “Plan of Action for Strengthening Information Systems for Health 2019-2023,” 2019.
[28] World Health Organization, “Digital Implementation Investment Guide (DIIG),” 2020.
[29] World Health Organization, “Digital Implementation Investment Guide (DIIG),” 2020.
[30] World Health Organization, “Digital Implementation Investment Guide (DIIG),” 2020.
[31] World Health Organization, “Digital Implementation Investment Guide (DIIG),” 2020
[32] World Health Organization, “Smart Guidelines”, 2021.
[33] World Health Organization, “Digital Health Platform Handbook: Building a Digital Information Infrastructure (Infostructure) for Health,” 2020.
[34] World Health Organization, “Digital Health Platform Handbook,”2020.
[35] PATH, “Product Vision for the Better Immunization Data (BID) Initiative,” PATH, 2014.
[36] World Health Organization, “Budget and Financing: Financial Flow,” Last modified Feb 1, 2020.
[37] “Digital Investment Principles,” Last modified May 12, 2018.





