Task Force 6 Accelerating SDGs: Exploring New Pathways to the 2030 Agenda
Abstract
Universal digital access to inclusive healthcare is a part of the G20’s vision to achieve Sustainable Development Goal-3 (good health and well-being), but the pathways to accomplish this are unspecified. India and other countries are in the process of extensively digitalising healthcare. This policy brief provides a roadmap to integrate the digital healthcare infrastructure for affordable, equitable, and universal access. The roadmap is presented using an ontology of universal digital access to inclusive healthcare. Policies related to universal digital access to inclusive healthcare must be based on the large number of pathways encapsulated in the ontology. The known effective pathways to universal digital access to inclusive healthcare must be reinforced, the known ineffective pathways must be redirected, and the unknown new pathways that must be discovered and explored.
The Challenge
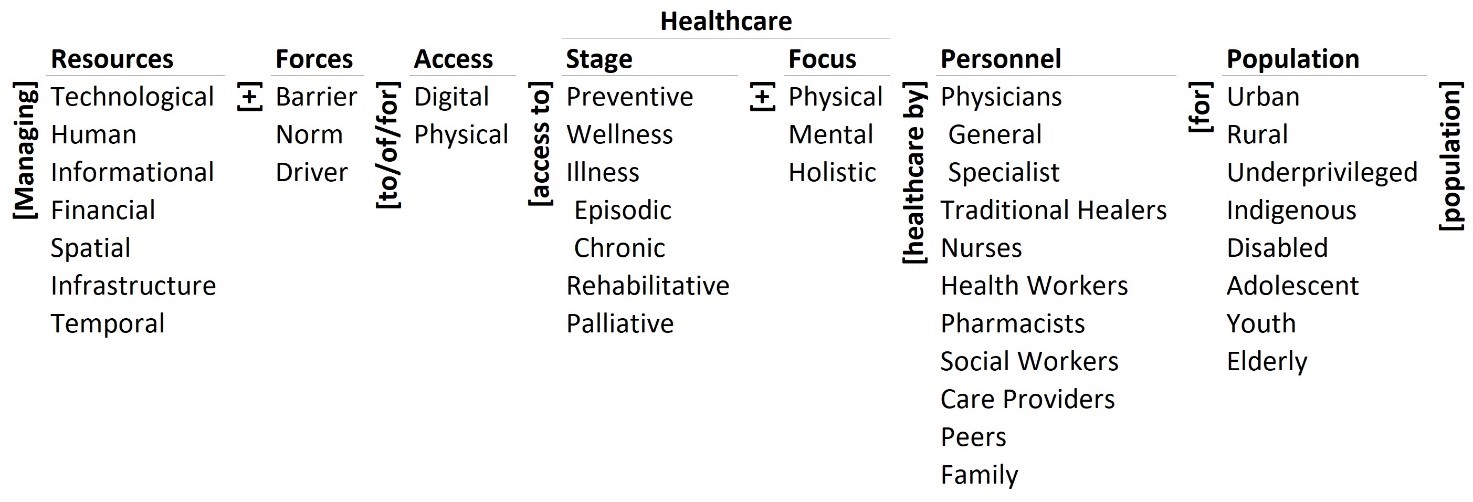
Universal digital access to inclusive healthcare is part of India’s and the G20 countries’ Sustainable Development Goal-3 (SDG-3) vision. The challenge of such access is complex and must be defined. Its ontology (see Figure 1[a]) is a clear, concise, and comprehensive definition of the complexity, and a ‘map’ of the pathways to meet the challenge.
Ontology of universal digital access to inclusive healthcare
When defining ‘universal digital access to inclusive healthcare’, healthcare can be understood as: (a) physical, mental, and holistic care, and (b) preventive, wellness, illness (episodic, chronic), rehabilitative, and palliative care. These elements are listed as the focus and stage of healthcare in the ontology (Figure 1). Thus, the 6*3 = 18 combinations of focus and stage that denote healthcare include, for example, (a) preventive physical healthcare, and (b) rehabilitative mental healthcare. As such, healthcare policies must address the requirements for these 18 combinations for all population segments.
Digital access must be blended with physical (in-person) access for the delivery of inclusive healthcare. The care must be delivered by a range of personnel, including physicians (generalists and specialists), traditional healers, nurses, health workers, pharmacists, social workers, care providers, peers, and the family. Thus, access to healthcare denotes 2*6*3*10 = 360 possible combinations that include, for example, (a) digital access to preventive physical healthcare by health workers, and (b) physical access to rehabilitative mental healthcare by care providers. The policies must address the requirements for these 360 combinations for all population segments.
Universal access to inclusive healthcare denotes access for all the population segments: urban, rural, underprivileged, indigenous, disabled, adolescent, youth, and the elderly. The requirements of and the services provided to these segments must be differentiated and integrated for effective healthcare. Thus, universal access to inclusive healthcare denotes 2*6*3*10*8 = 2,880 combinations that include, for example, (a) digital access to preventive physical healthcare by health workers for urban population, and (b) physical access to rehabilitative mental healthcare by care providers for the indigenous population. The policies must address the requirements for these 2,880 combinations for all population segments.
Figure 1: Ontology of Universal Digital Access to Inclusive Healthcare
Source: Authors’ own
The three types of forces affecting the delivery of universal access to inclusive healthcare are listed in the second column of the ontology. They are: (a) barriers to, (b) norms for, and (c) drivers of access. Thus, the forces determining access are: 3*2*6*3*10*8 = 8,640, and include, for example, (a) barriers to digital access to preventive physical healthcare by health workers for the urban population, and (b) norms for physical access to rehabilitative mental healthcare by care providers for the indigenous population. The policies must be based on the knowledge of these 8,640 forces.
The policies must: (a) remove the barriers to providing these types of care, and (b) establish norms for providing them, and (c) introduce drivers of the same by managing the seven types of resources (technological, human, informational, financial, spatial, infrastructure, and temporal resources). Thus, there are 7*3*2*6*3*10*8 = 60,480 possible pathways to universal digital access to inclusive healthcare encapsulated in the ontology that include, for example, (a) managing technological barriers to digital access to preventive physical healthcare by health workers for the urban population, and (b) managing financial norms for physical access to rehabilitative mental healthcare by care providers for the indigenous population.
Countries can systematically choose pathways for universal digital access to inclusive healthcare based on the ontology and formulate policies to implement them. The choice and the formulation must be based on the best available evidence from research, other policies, and practice. The ontological analysis will thus provide a comprehensive roadmap to formulate effective policies for universal digital access to inclusive healthcare in India and the G20 countries.
The G20’s Role
The G20 can play a key role in addressing the challenge of providing universal digital access to inclusive healthcare by establishing a committee to set an agenda for: (a) research, policy, and practice, and (b) translation of research to policy to practice through feedback and learning. At present, there is no similar unified framework or concerted effort to address the challenge and provide a roadmap. The committee’s agenda must inform and be informed by the constituent country agendas, and those of the United Nations (UN) and its agencies, the World Health Organization (WHO), and others.
The ontology of universal digital access to inclusive healthcare must be adopted as a framework for all G20 countries. Within the framework, each country must choose its pathways based on its local requirements, priorities, and resources. The adoption of a common framework will help formalise and transfer knowledge about, and feedback and learnings from the implementation within a country to other G20 and non-G20 countries. Such an approach will help move the cycle of generating and applying knowledge on the challenge from a selective, segmented, and siloed effort to a synoptic, systemic, and systematic one.
The framework must be used to periodically map the state-of-the-art, state-of-the-need, and state-of-the-practice of universal digital access to inclusive healthcare by country. Analysing the gaps between the three states must guide the translation of research to policy to practice and then back to research for feedback and learning to achieve the SDG-3 vision. As such, the G20 committee must help the member countries collaborate, coordinate their policies, and communicate their learning.
Recommendations to the G20
The G20 must form an international committee and encourage the creation of national groups, for universal digital access to inclusive healthcare. These committees must adapt and adopt the ontology as a common framework, and pursue a systemic approach that harnesses the resources and unleashes the forces necessary to deliver such care. These committees must be responsible and accountable for the outcomes. The detailed recommendations to the G20 are organised by the columns of the ontology and then integrated. These recommendations are aligned with the present research, policies, practices, and recommendations of the WHO, UN agencies, and other similar bodies. Their prioritisation must be country specific.
Digital healthcare
The digital healthcare policy priorities must be aligned with, adapted to, and shape each country’s healthcare priorities.
- Physical healthcare will continue to be important; mental healthcare is becoming more important; and holistic healthcare is gaining importance (for instance, in India). Digital access must differentiate between and integrate the requirements of these focuses of care.
- The priorities of the different stages of care change with advances in medical knowledge, country demographics, requirements of the population, and the country’s healthcare policies. Digital access must longitudinally integrate and support the requirements of different stages of care, from pre-conception to death.
- Digital healthcare must be integrated, people-centred, interoperable, and with high fidelity.
- Digital access to healthcare should help generate data to determine the most effective and efficient interventions for inclusive healthcare of a country’s population.
- It should end drudgery and repetitive work, eliminate paperwork, help make better decisions, and offer guidelines to health workers to improve adherence to clinical guidelines.
- Digital healthcare governance must be aligned with the country’s healthcare governance structure and legal requirements.
Digital healthcare access
Digital access is necessary but not sufficient for effective and efficient healthcare. It must be symbiotic with physical (in-person) access to healthcare. The capabilities of the combination must be harnessed systematically.
- Digital access to healthcare must complement, supplement, or substitute physical (in-person) access as necessary and appropriate for all stages and focuses of healthcare.
- Digital and physical (in-person) access must be balanced based on the healthcare requirements, personnel delivering it, and the population receiving it.
- Digital access to healthcare must address the new challenges of communication, compliance, adherence, motivation, and behaviour.
- Digital healthcare access and engagement must be proactive and not reactive. It must transform the scale and scope of healthcare by harnessing the power of digitalisation, and not simply satisfy the present requirements and automate the present delivery.
- Digital healthcare access must be equitable and must reduce the disparities in healthcare.
Digital healthcare delivery personnel
Digital access must be available to the full spectrum of healthcare providers based on their role, requirements, and the need they satisfy. It must help automate, ‘informate’,[b] and then transform their role in healthcare delivery.
- Digital access for a person’s healthcare delivery must be transferable across healthcare providers during the lifecycle of care and the person’s lifetime.
- Digital access must be able to deliver disease-specific programmes and patient-centric care effectively.
- Digital access for a person’s healthcare delivery must be trusted, private, confidential, and secure.
- Digital access for a person’s healthcare delivery must support and integrate the specialised healthcare functions of the different providers.
- Digital access for a person’s healthcare delivery must be included in the curriculum, training, and competencies.
Digital healthcare recipient population
Digital access must be available to all population segments based on their requirements, needs, location, and resources. These must be mapped in detail. The access must adapt to the changing requirements and needs as the populations learn and their expectations evolve. It must address the benefits and challenges of such access for different population segments.
- The provision of digital access to healthcare must be mass-customised to the populations based on their requirements, location, and resources.
- The people belonging to the population segments must be partners in the design, development, and delivery of digital access to healthcare. Their cultural sensitivities must be part of the process.
- Feedback and learning from the populations on digital access to healthcare must result in the simultaneous globalisation and localisation of access.
- Universal digital access to inclusive healthcare must be delivered to all population segments based on their priorities and needs. In the future, their priorities and needs may change significantly because of digital access to healthcare. The feedback must be factored into the policies.
- Aggregate data must be made available to researchers and policymakers to assess the effectiveness of programmes and interventions.
Digital healthcare forces
Digital access to healthcare policies must establish norms for such access, help overcome the barriers to access, and aid the drivers of the same. However, sometimes, some barriers may be introduced and drivers removed to ensure the legality and conformance of healthcare delivery.
- Governance, legal, and regulatory policies must establish norms for digital access to healthcare.
- The ethics of digital healthcare delivery and receipt must be normalised.
- Resources must be deployed to enforce the governance, legal, regulatory, and ethical norms even at the cost of enhancing the barriers and diminishing the drivers.
- Resources must be deployed to overcome barriers to digital access to healthcare. These barriers may include quality of connection, frequent updates to operating systems and platforms, and personnel fatigue.
- Resources must be deployed to support drivers of digital access to healthcare. These drivers may include education, hand holding, incentives, and operation flexibility.
Digital healthcare resources
Technological and financial resources are necessary but not sufficient for universal digital access to inclusive healthcare. The full spectrum of resources in the ontology must be managed to drive universal digital access to inclusive healthcare, conform to the norms, and to overcome the barriers.
- Technological resources must be accessible to the personnel delivering care and the population receiving it. It must be available for all stages and focuses of healthcare. It must meet the quality requirements of all users.
- Human resources must design, develop, and operate the system effectively and efficiently. It must support the functions of the technology for the personnel delivering care and the population receiving it. It must also support the functions for all stages and focuses of healthcare. It must assure the quality of universal digital access to inclusive healthcare.
- Informational resources must informate and transform universal digital access to universal healthcare. The information must be about the system, managed by the system, and applied to the system. The information must include that about the population receiving healthcare, the personnel providing it, the different stages of healthcare, and the different focuses. It must provide support for transactions, decisions, interpretation, and knowledge development.
- Financial resources underpin the availability, accessibility, and quality of all the other resources and, consequently, of the system. They must also ensure the continuity of the system across locations and over time—the two key advantages of digital access over physical (in-person) access.
- Spatial resources must be available and accessible for the healthcare personnel and the recipients to maintain the confidentiality, privacy, and security of their interaction. They are needed at both ends for the technology and other infrastructure required for universal digital access to inclusive healthcare. The spatial resources may be independent of that for physical (in-person) access to healthcare or collocated with it.
- Infrastructure resources are non-technological physical resources, such as buildings, plumbing, administration, and other support systems. They are not directly in the path of healthcare delivery but support the personnel delivering and population receiving it.
- Temporal resources help match the availability and accessibility of the healthcare personnel and recipients. They also assure the provision of episodic (any time) emergency healthcare services as well as the ongoing (any duration) regular services.
Universal digital access to inclusive healthcare
The success in providing universal digital access to inclusive healthcare will depend on its governance locally, nationally, and globally by the proposed committees. In addition to formulating policies, governance must include the mission of generating knowledge and applying it through formal research and assessment of policies and practices. It must be aligned and integrated with the country’s digital health mission, and utilise the ecosystem created by such a mission effectively. Each country must develop an ongoing learning system with feedback to guide the trajectory of universal digital access to inclusive healthcare.
Conclusion
Achieving universal digital access to inclusive healthcare requires a roadmap. This policy brief provides a clear, concise, and comprehensive framework to negotiate the labyrinth of pathways. The framework can be used for the governance of systems to provide such access locally, nationally, and globally. It can be the basis of a learning healthcare system. Further, in many low-income countries there is a substantial need for technology sponsors and financial resources. Every country should assess its current strategies and coordination mechanisms. Universal digital access will benefit from stronger legal bases and adequate capacity building to set up infrastructure that drives the digital transformation process, strengthening institutional frameworks and mechanisms that enhance efficiencies and improve service delivery.
Attribution: Arkalgud Ramaprasad et al., “Pathways to Universal Digital Access to Inclusive Healthcare in the G20,” T20 Policy Brief, May 2023.
Bibliography
Select Literature on Digital Access to Healthcare
Asian Development Bank. “Guidance for Investing in Digital Health,” 2018.
Federation of Indian Chambers of Commerce and Industry. “Re-Engineering Indian Healthcare 2.0,” 2019.
Garrett Mehl, Özge Tunçalp, Natschja Ratanaprayul, Tigest Tamrat, María Barreix, David Lowrance, Kidist Bartolomeos, et al. “WHO SMART Guidelines: Optimising Country-Level Use of Guideline Recommendations in the Digital Age.” The Lancet Digital Health 3, no. 4 (April 1, 2021): e213–16.
International Telecommunication Union News. “Digital Systems Support Equitable Healthcare.” ITU Hub, March 17, 2022.
Ministry of Health and Family Welfare. “Health Data Management Policy.” Government of India, 2020.
———. “National Digital Health Blueprint,” 2019.
National Health Authority. “National Digital Health Mission.” Ministry of Health and Family Welfare, Government of India, July 2020.
National Health Service, England. “A Plan for Digital Health and Social Care.” GOV.UK, 2022.
NITI Aayog. “National Health Stack: Strategy and Approach.” Government of India, July 2018.
———. “Public Health Surveillance in India 2035,” 2020.
Shoshana Zuboff. In The Age Of The Smart Machine: The Future Of Work And Power. New York: Basic Books, 1988.
United Nations. “Secretary-General’s Roadmap for Digital Cooperation,” 2020.
World Health Organization. “Global Diffusion of EHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on EHealth,” 2016.
———. “Global Strategy on Digital Health 2020-2025,” 2021.
———. How to Plan and Conduct Telehealth Consultations with Children and Adolescents and Their Families. Geneva: World Health Organization, 2021.
———. “Recommendations on Digital Interventions for Health System Strengthening,” 2019.
———. “Young People and Digital Health Interventions: Working Together to Design Better,” 2020.
Authors’ Selected Publications
Adrian P. Mundt, Matías Irarrázaval, Pablo Martínez, Olga Fernández, Vania Martínez, and Graciela Rojas. “Telepsychiatry Consultation for Primary Care Treatment of Children and Adolescents Receiving Child Protective Services in Chile: Mixed Methods Feasibility Study.” JMIR Public Health and Surveillance 7, no. 7 (July 22, 2021): e25836.
Alicia Núñez, Arkalgud Ramaprasad, Thant Syn, and Harold Lopez. “An Ontological Analysis of the Barriers to and Facilitators of Access to Healthcare.” Journal of Public Health, April 5, 2020.
Alicia Núñez, S. D. Sreeganga, and Arkalgud Ramaprasad. “Access to Healthcare During Covid-19.” International Journal of Environmental Research and Public Health 18, no. 6 (March 14, 2021): 2980.
Álvaro Jiménez-Molina, Pamela Franco, Vania Martínez, Pablo Martínez, Graciela Rojas, and Ricardo Araya. “Internet-Based Interventions for the Prevention and Treatment of Mental Disorders in Latin America: A Scoping Review.” Frontiers in Psychiatry 10 (2019).
Ariel I La Paz and Arkalgud Ramaprasad. “Aligning Biomedical Informatics with Clinical and Translational Science.” In Proc. Ann. Hawai’i Int. Conf. Syst. Sci., HICSS, 2009.
Arkalgud Ramaprasad, Annette L Valenta, and Ian Brooks. “Clinical and Translational Science Informatics: Translating Information to Transform Health Care.” In HEALTHINF – Proc. Int. Conf. Hlth. Informatics, 135–41, 2009.
Arkalgud Ramaprasad, Nanda Kumar Bidare Sastry, and Thant Syn. “Envisioning Precision Healthcare Informatics: A Unified Framework.” In MEDINFO 2017: Precision Healthcare through Informatics, 245:564–68. IOS Press, 2017.
Arkalgud Ramaprasad, Shobana Gupta, Sridhar R Papagari Sangareddy, A. Prakash, and R. Venkatasubramanian. “Bridging the Digital Divide in E-Health Applications: Leading the Way to an Informed Patient.” International Journal of Healthcare Technology and Management 8, no. 1–2 (2007): 120–40.
Arkalgud Ramaprasad, Sridhar S Papagari, and Joy Keeler. “EHealth: Transporting Information to Transform Health Care.” In HEALTHINF – Proc. Int. Conf. Hlth. Informatics, 344–50. Porto, Portugal, 2009.
Arkalgud Ramaprasad, Susanna Ghosh Mitra, Devina Neogi, S D Sreeganga, and Nibras K Thodika. “Integration of Data Science for Timely Tuberculosis (TB) Care.” TBINFO 2, no. 1 (March 2022).
Graciela Rojas, Vania Martínez, Pablo Martínez, Pamela Franco, and Álvaro Jiménez-Molina. “Improving Mental Health Care in Developing Countries Through Digital Technologies: A Mini Narrative Review of the Chilean Case.” Frontiers in Public Health 7 (2019).
Joshua D. Cameron, Arkalgud Ramaprasad, and Thant Syn. “An Ontology of and Roadmap for MHealth Research.” International Journal of Medical Informatics 100 (April 2017): 16–25.
Nibras K Thodika, Susanna Ghosh Mitra, Arkalgud Ramaprasad, and Sulegai Dhondusa Sreeganga. “Toward Strengthening Active Case Finding for Ending Tuberculosis in India.” International Journal of Health Planning and Management, August 21, 2021, 1–6.
Pablo Martínez, Graciela Rojas, Vania Martínez, María Asunción Lara, and J. Carola Pérez. “Internet-Based Interventions for the Prevention and Treatment of Depression in People Living in Developing Countries: A Systematic Review.” Journal of Affective Disorders 234 (July 1, 2018): 193–200.
Suman Gadicherla, Lalitha Krishnappa, Bindu Madhuri, Susanna G. Mitra, Arkalgud Ramaprasad, Raja Seevan, S. D. Sreeganga, Nibras K. Thodika, Salu Mathew, and Vani Suresh. “Envisioning a Learning Surveillance System for Tuberculosis.” PLOS ONE 15, no. 12 (December 14, 2020): e0243610.
Vania Martínez, Marcelo A. Crockett, Ajay Chandra, Sarah Shabbir Suwasrawala, Arkalgud Ramaprasad, Alicia Núñez, and Marcelo Gómez-Rojas. “State of Mental Health Research of Adolescents and Youth in Chile: An Ontological Analysis.” International Journal of Environmental Research and Public Health 19, no. 16 (2022): 9889.
[a] The ontology in Figure 1 has been developed based on the extensive experience of the authors and selected literature.
[b] To informate is to generate information about healthcare delivery and make it visible.





