TF-6: Accelerating SDGs: Exploring New Pathways to the 2030 Agenda
The COVID-19 pandemic wreaked havoc across the world, causing more than 660 million reported cases and 6 million deaths in three years. Since 2000, other pathogens, including the 2002 SARS, 2013 Ebola, 2014 Bird Flu, 2015 MERS, and 2022 Monkeypox have recorded serious outbreaks varying in severity. Pre-existing rules and regulations, such as the International Health Regulations, have failed to efficiently detect the outbreaks and effectively contain their spread. This Policy Brief discusses the formation of G20-led early warning, detection, and response teams to disease outbreaks. These teams would be based in select member nations and have the expertise to collect data and identify emerging health threats. After the detection of a threat, the G20 should help the affected country with accelerated access to financial resources.
1. The Challenge
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, emerged in Wuhan, China, in late 2019 and spread rapidly across the world. As of July 2023, there have been over 768 million confirmed cases and nearly 7 million deaths worldwide.[1]
The pandemic has had significant impacts on daily life, including widespread lockdowns, travel restrictions, and the closure of businesses and schools. The pandemic also adversely affected the global economy, with many countries experiencing significant economic downturns.
The pandemic highlighted significant disparities in access to healthcare and resources, with marginalised communities and low-income countries being disproportionately affected.[2] The repercussions include stresses on mental health, with many people experiencing increased anxiety and depression.[3] There are also concerns about emerging variants of the virus and possible emerging pathogens, which could spread all over (Figure 1 shows some of the notable pathogens that were detected in the 21st century.)
Figure 1: Notable Epidemics Since 2000
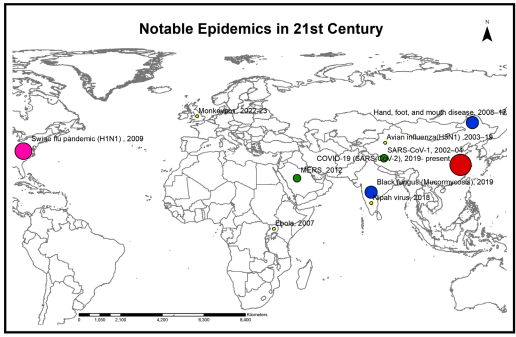
Note: The map shows the countries of detection, which can be different from the countries of origin. The size of the circle is indicative of the number of deaths caused by that particular epidemic. The positions on the map are not exact and are only representational.[4]
- Increased encroachment on natural habitats and ecosystems. This exposes humans to new pathogens. As populations expand and encroach on wild areas, there is more human–animal interaction leading to an increase in the emergence of new pathogens.
- Climate change. Changes in temperature and precipitation patterns affect the distribution of vector-borne diseases, such as malaria and dengue fever.
- Inappropriate use of antibiotics and other antimicrobial agents in agriculture and healthcare. This has led to the development of antibiotic-resistant organisms, which are causing severe health consequences in conditions which were previously effectively treatable.
While these factors affect the emergence of new pathogens, the increased interconnectedness of the world facilitates their spread. (Figure 2 points out the potential hotspots of novel pathogens. This can help determine areas that should be placed under increased surveillance.)
Figure 2: Potential Hotspots of Novel Pathogens
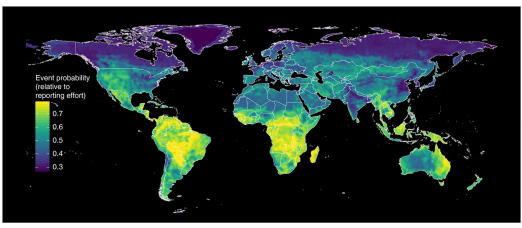
Source: ‘Global hotspots and correlates of emerging zoonotic diseases.’[5]
- Lack of funding. Setting up and maintaining effective surveillance and response systems can be expensive, and many countries may lack the necessary resources to invest in these efforts. For example, the Centers for Disease Control in the United States, works in coordination with local and state health departments and facilities to maintain its early detection systems. The US government recently awarded the centre US$2.1 billion to strengthen its network over the next few years. This points to the enormous resources that are required to maintain such a system.[6]
- Limited healthcare infrastructure. In low-income countries, healthcare systems may be under-resourced and ill-equipped to respond to emerging infectious diseases.
- Lack of coordination. There is often a lack of coordination and cooperation among countries and international organisations in sharing information and resources. This can hinder global response to a novel pathogen. Effective surveillance and coordinated response require close collaboration between different sectors, agencies, and countries.
- Lack of political will. The potential consequences of a pandemic are often perceived as too distant or uncertain to motivate immediate action. There is often a lack of political will to invest in preparedness as it may not provide tangible benefits until a crisis occurs. Without political will, it is difficult to invest in and prioritise efforts.
- Limited technical expertise. Setting up and maintaining effective surveillance and response systems requires specialised technical expertise, which may be lacking in some countries.
There are a number of existing global systems which failed in the timely detection of COVID-19 because of inadequate resources, wide scope of mandate, and lack of prioritisation by political systems.
a. WHO’s International Health Regulations (IHR)
It is a legally binding instrument signed by 196 countries. IHR makes it compulsory for countries to follow a set of rules and regulations, to detect, report, and respond to public health emergencies. IHR has been criticised for lack of enforcement and imposition of penalties for non-compliance. In the emergence of COVID-19, China flouted IHR rules and did not report COVID-19 cases within the required time.[7]
b. Global outbreak alert and response network (GOARN)
GOARN is a global system established by the World Health Organization (WHO) in 2000 to respond to and control outbreaks of infectious diseases. GOARN brings together technical expertise and resources from a number of international organisations, including UN agencies, non-government organisations (NGOs), and academic institutions. They respond with deployment of staff and resources to affected countries. However, GOARN does not have the required resources to tackle the problem.[8]
c. Force Health Protection Agency of NATO and MediSys of EU are similar mechanisms
The current surveillance systems of international or national organisations have certain limitations made apparent by COVID-19. The main problem with international organisations like WHO is that they depend on the generosity of a ‘host’ country to access ground-level as well as collated data from that country. The limitation of national systems is that domestic compulsions or budgetary constraints can influence the efficiency of their monitoring systems. For example, the Global Public Health Intelligence Network, arguably the best monitoring system in the world, did not detect the COVID-19 outbreak due to the different priorities of the Canadian government, which was to focus on domestic health matters.[9] The current systems have not worked effectively over and over again, including in the early detection of SARS, Ebola, and COVID-19.[10]
To achieve Sustainable Development Goals (Goal 3, target 3.d, which is on strengthening the capacity of all countries, in particular developing countries, for early warning, risk reduction, and management of national and global health risks), averting future epidemics and pandemics is important. However, it is apparent that the lead on this should be taken by a multilateral group, smaller than behemoths like WHO and stronger than individual nations. The G20 is a natural fit in this scenario: it has the necessary resources to set up this multilateral group; is home to the majority of the world’s population; and because historically various members, such as China and Saudi Arabia, are at an increasing risk of witnessing the emergence of new pathogens.
2. The G20’s Role
The G20 should create a system for early detection and response to potential pathogens that can become dangerous as they can easily spread across borders. Therefore, an early warning and response system is crucial for global health security as the system could help build the capacity of countries to detect and respond to infectious disease outbreaks and even facilitate the prevention of pandemics before they occur.
The G20 countries are better placed to lead the system for they are the largest and most influential economies in the world and have significant resources at their disposal. This includes the financial means to invest in necessary capacity building. They also have the political power and influence to drive global cooperation and coordination. They can easily mobilise international resources, coordinate global response efforts, and provide financial and technical assistance to countries that require them. Some of the G20 countries (for instance, the European Union, and the US) have well-established public health systems and infrastructure, which can be leveraged to support the proposed system.
By establishing a system for early detection of pathogens, the G20 can demonstrate its commitment to global health security.
3. Recommendations to the G20
The G20 must consider the following.
a. Formation of a G20-led early warning, detection and response (GEWDR) team for disease outbreaks.
The GEWDR should be established:
- At the national level of select G20 nations.
- At the G20 level.
These teams would have the mandate to develop and implement rapid response plans for emerging infectious diseases, epidemics, and pandemics. The teams should be interdisciplinary, and consist of experts like epidemiologists, microbiologists, data analysts, and public health professionals. They should work in collaboration with national public health agencies and WHO to monitor, identify, and respond to potential outbreaks of infectious diseases. The teams would be responsible for the early detection of outbreaks, the rapid deployment of response teams, and the coordination of local and international response.
The G20 countries should also play a crucial role in supporting other countries set up their national teams, and creating a network of experts and resources that would be critical in preventing and controlling future pandemics.
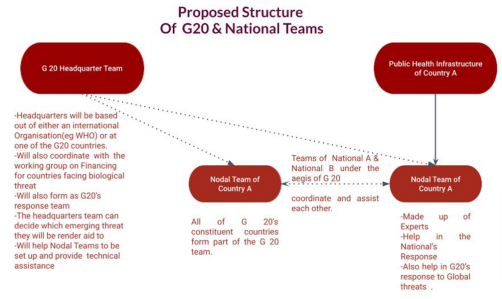
Figure 3: Proposed Structure of the G20 and National Teams
The teams would be situated in select G20 nations and made responsible for monitoring and responding to infectious disease outbreaks within their respective countries. The teams could work at three levels. The first level would be a global digital monitoring system to monitor digital content on biological events. The teams could use technologies like artificial intelligence, auto-translation, and sentiment analysis to create a real-time scenario of an emerging situation.
Level two would consist of a permanent staff of public health professionals, statisticians, epidemiologists, as well as analysts trained in strategic studies. At this level, any emerging biological event would be analysed using a threat matrix that considers biological as well as strategic inputs to safeguard the G20’s interests. Level three should have trained personnel to collect samples directly from the field so as to cross-validate data coming from other sources.
Relation between national teams and G20 headquarters
G20 headquarters would be responsible for coordinating with the different nodal teams. The headquarters would provide strategic direction to the teams as well as give technical and logistical support. In addition, the nodal teams would be expected to share information and best practices and to collaborate on the development of new tools and technologies for infectious disease surveillance and response.
G20 headquarters would monitor the progress and effectiveness of the national teams. They could establish a system for regular reporting and evaluation and present the findings as part of each G20 summit. The G20 and individual countries could use this information to identify areas that require improvement. The headquarters would also use the data collected to develop a better understanding of the global disease landscape and make decisions about resource allocation and policy interventions.
G20 countries could also share their experiences and best practices with other countries in the African Union and ASEAN to help them set up their teams. This approach would enable the G20 countries to build a network of teams worldwide, creating a coordinated and effective response to pandemics. The teams would also be part of a global response team to tackle any new health threat around the globe. The global team and headquarters could be situated at WHO or in one of the G20 countries.
b. Accelerating access to financing for countries tackling a new threat
Despite the best efforts at surveillance, it is possible that a new pandemic may manifest itself. There are several possible efficient ways for the G20 to provide financing to countries if a new pandemic emerges.
- Emergency fund. To establish an emergency fund that G20 countries could quickly tap into to finance countries facing paucity of funds. This fund could be established before a pandemic, with contributions from G20 countries and could be used to provide immediate funding to countries that require it. A similar initiative by WHO called the Pandemic Fund is being set up. However, it has been considerably criticised for merely repurposing existing global health funds.[11]
- Contingency planning. The G20 can help its members develop contingency plans for financing a pandemic. These plans could include pre-agreed financing mechanisms, as well as emergency loans or grants that could be activated quickly in an outbreak.
- Coordination with multilateral institutions. The G20 could also work closely with institutions like the World Bank, and the International Monetary Fund (IMF) to provide financing. These institutions already have financing mechanisms in place, and could be used to provide funding quickly to countries that lack funds.
Overall, the key to providing quick financing for a pandemic is to have pre-existing mechanisms that can be activated promptly. The G20 could play an important role in developing and coordinating these mechanisms to ensure that countries have access to quick finance to swiftly respond to emerging pandemics.
The G20 should establish a working group to oversee the distribution of emergency financing. The allocation of funds should depend on factors like the scope and severity of the pandemic, and the resources and capabilities available. It must be ensured that emergency financing swiftly reaches those who require it the most, and that the funds are used effectively to mitigate the effects of the outbreak. This working group therefore should include experts from fields like public health, economics, and finance.
It is important to ensure that the working group operates in a transparent and impartial manner. The allocation of emergency financing should be based on objective criteria, such as the severity of the outbreak, the country’s capacity to respond, and the potential impact on global health and economy.
Attribution: Harshit Kukreja and Shambhavi Naik, “Global Teams for Early Warning, Detection, and Response to Disease Outbreaks,” T20 Policy Brief, July 2023.
Endnotes
[1] World Health Organisation. WHO Coronavirus (COVID-19) Dashboard. Last accessed on July 25, 2023. https://covid19.who.int/
[2] Akihiko Nishio, “Covid-19 Is Hitting Poor Countries the Hardest. Here’s How World Bank’s Ida Is Stepping up Support,” World Bank Blogs, January 28, 2021, https://blogs.worldbank.org/voices/covid-19-hitting-poor-countries-hardest-heres-how-world-banks-ida-stepping-support.
[3] Jiaqi Xiong, Orly Lipsitz, Nasri Flora, Leanna MW Lui, Hartej Gill, Lee Phan, David Chen-Li, Michelle Lacobucci, Roger Ho, Amna Majeed et al., “Impact of COVID-19 pandemic on mental health in the general population: A systematic review,” Journal of affective disorders 277 (2020): 55-64, doi: 10.1016/j.jad.2020.08.001.
[4] Rita, Meganck, and Ralph, Baric. Developing therapeutic approaches for twenty-first-century emerging infectious viral diseases. Nat Med 27, 401–410 (2021). https://doi.org/10.1038/s41591-021-01282-0
[5] Toph Allen, Kris A. Murray, Carlos Zambrana-Torrelio, Stephen S. Morse, Carlo Rondinini, Moreno Di Marco, Nathan Breit, Kevin J. Olival, and Peter Daszak, “Global hotspots and correlates of emerging zoonotic diseases,” Nature communications 8, no. 1 (2017): 1124.
[6] Centers for Disease Control and Prevention. “CDC to invest $2.1 billion to protect patients and healthcare workers from COVID-19 and future infectious diseases.” (2021).
[7] Sam Halabi and Kumanan Wilson, September 2. “Evaluate China’s Pandemic Response Using International Health Regulations.” Policy Options, April 6, 2021.
[8] Bill Gates, “Meet the Germ Team,” GatesNotes, April 30, 2022, https://www.gatesnotes.com/Meet-the-GERM-team.
[9] Robertson, Grant. “Without early warning you can’t have early response”: How Canada’s world-class pandemic alert system failed.” Globe and Mail 25 (2020).
[10] Dennis Carroll, Subhash Morzaria, Sylvie Briand, Christine Kreuder Johnson, David Morens, Keith Sumption, Oyewale Tomori, and Supaporn Wacharphaueasadee, “Preventing the next pandemic: the power of a global viral surveillance network,” BMJ, March 12, 2021, https://www.bmj.com/content/372/bmj.n485.
[11] Garrett Wallace Brown, Tacheva Blagovesta, Shahid Minahil, Natalie Rhodes, and Marco Schäferhoff, “Global Health Financing after COVID-19 and the New Pandemic Fund,” Brookings, December 7, 2022, https://www.brookings.edu/blog/future-development/2022/12/07/global-health-financing-after-covid-19-and-the-new-pandemic-fund/.