TF 3: LiFE, Resilience, and Values for Well-being
The pandemic-triggered global crisis has led to the need for an international and holistic approach to pursue ‘health security and wellbeing for all’ that addresses social, economic, environmental, and spiritual elements. To fulfil this global task by fostering the efficient implementation of solutions, the G20 should promote international collaborations in finance, technology, capacity building, and interoperability of solutions. Building on the G20’s endorsement of the One Health approach, member economies should adopt partnerships in wellbeing, as well as curative, preventive, and promotive healthcare initiatives. Interoperability needs to be integrated at multiple levels into the solutions emerging from these partnerships, especially since effective, efficient, and expeditious implementation of coordinated responses have become inevitable, given the cross-border nature of risks associated with wellbeing.
1. The Challenge
Lessons from the pandemic: Towards a more integrated and holistic approach to healthcare
Healthcare systems globally, and particularly in the Global South, faced tremendous strain following the COVID-19 outbreak (Uwishema et al. 2022). The ‘new normal’ is witnessing an increase in demand for strengthening healthcare infrastructure to cater to wellbeing. Inadequacies in different medical systems have necessitated integrative and innovative approaches (e.g., COVAX initiative, GAVI COVAX AMC, ACT-Accelerator, etc.). Comprehensive public health measures and norms aimed at addressing the related international problems, risks, and challenges are now considered a global public good (Hein 2020).
The World Health Organisation’s (WHO) 2021 Geneva Charter for Well-Being lays the foundation for the definition of inclusive and sustainable wellbeing covering various elements, including physical, mental, environmental, spiritual, and social wellbeing (WHO 2021). There is now global recognition for a holistic perspective on wellbeing rather than a mere focus on physical health through the instrumentality of modern medicine (UNGA 2011; OECD, n.d.; WHO 2023). Hence, the idea of wellbeing acknowledges the interplay of the above-mentioned elements and the concept of the G20-endorsed ‘One Health’ (See WHO 2023; G20 2022a).
Wellbeing and traditional medicine as complements to modern medicine
The G20 discussions have focused on methodologies where health, wellbeing, human development, and economic prosperity are seen as integral components of an optimally functional society. With health being central to every nation’s economic security, an ‘integrative healthcare’ approach, where traditional medicine (TM) is integrated alongside modern medicine, is being considered for policy actions (Government of India 2023a). The emphasis is on ‘value-based healthcare’ and holistic wellness. In this context, TM is key, since it is being used in more than 170 of the 194 WHO member states (with around 80 percent of the global population being TM users) (WHO 2022a). The combination of traditional and modern medicine with wellness treatments is also a G20 priority area (Government of India 2023b).
Moreover, traditional, complementary, and integrative medicine is critical to bridge the gap in regions where healthcare is expensive and difficult to access.[a] The WHO Traditional Medicine Strategy 2014-2023 is based on the fact that traditional therapies remain the primary source of health provision in many parts of the world (WHO 2013). There are over 40 African countries with national TM strategies and 34 TM research centres across 26 African countries. Nigeria is making efforts to standardise African TM. Further, herbal medicines are registered in 14 African countries, while 25 African countries have TM as part of their health science curricula (Bhattacharya 2023). James et al. (2020) note that TM is recognised in China and is part of its public healthcare system, where it is included in “insurance coverage, essential medicine list and is integrated with modern medical treatment facilities”.
In a number of countries, however, the cost of TM and treatments are not reimbursed under health insurance due to multiple reasons, including the lack of regulation on such medicines and practices (WHO 2019). Therefore, mutual recognition and optimisation is required to progress on a One Health journey (G20 2022b). There have been numerous efforts to overcome the chasm between traditional and modern medicine (see Table 1).
Table 1: Traditional Medicine (TM) Partnerships/Initiatives
| Traditional Medicine (TM) Partnership/Initiative | Aim |
| WHO-backed Global Centre for TM | Maximising the potential of TMs through modern science and technology |
| US-India Partnership on Cancer and TM Research | Boosting bilateral dialogue on TMs |
| MoU between All India Institute of Ayurveda and National Institute of Advanced Industrial Science and Technology, Japan | Promoting TM research and bridging the gap between research and commercialisation of TMs |
| MoU between Pharmacopoeia Commission for Indian Medicine & Homoeopathy and American Herbal Pharmacopoeia, USA | Developing standards and boosting the export potential of TMs |
| China-Australia International Research Centre for Chinese Medicine | High-impact research to support evidence-based healthcare |
Source: Authors’ own.
Wellbeing complementarities and interdependencies with health systems
Within the wider context of health and wellbeing, this Policy Brief adapts the work of Bastien-Olvera and Moore (2021) to highlight the interdependencies of health, food, and other systems with climate and the natural ecosystem as inputs to wellbeing (Figure 1).
Figure 1: The Conceptual Embeddedness of Health Systems and Wellbeing[b]
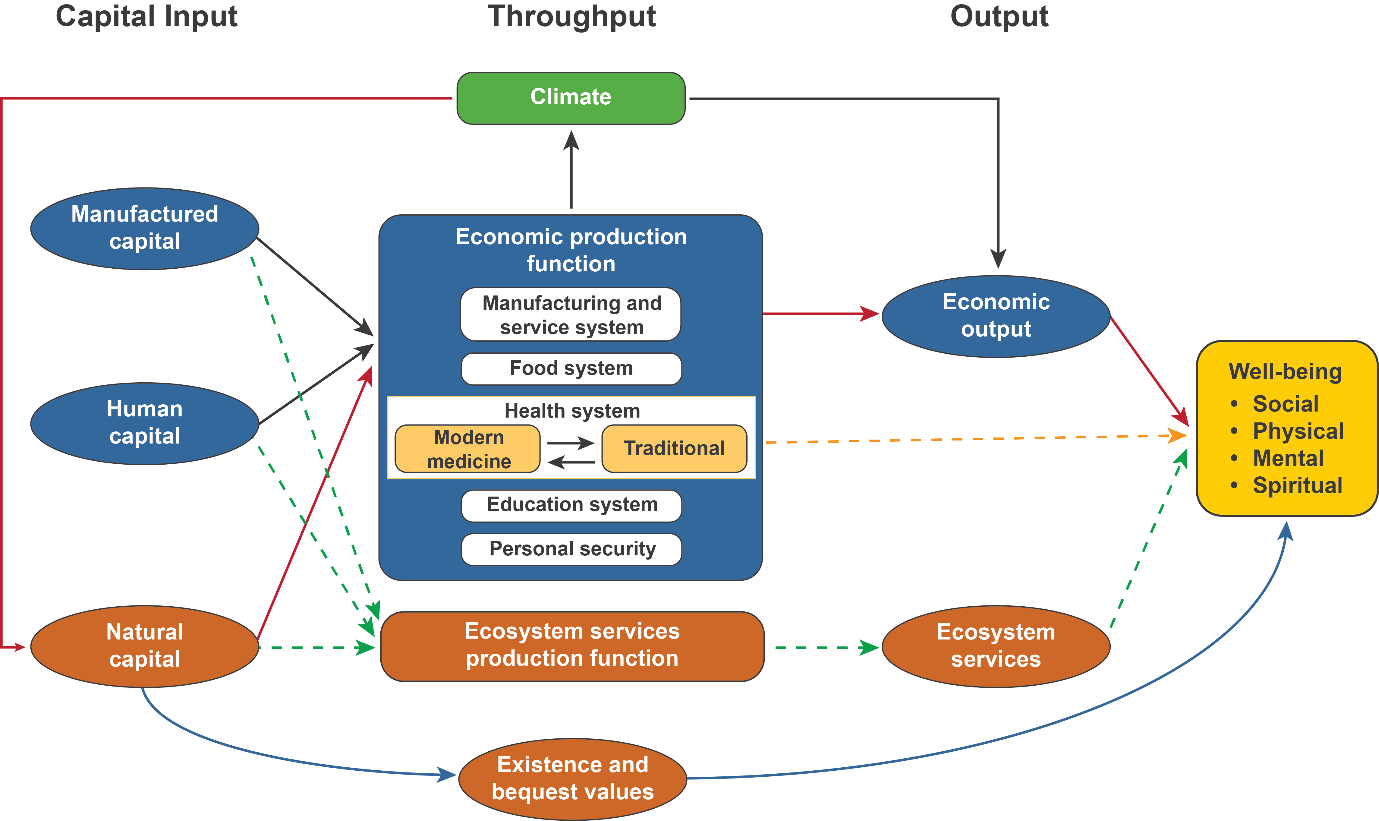
Source: Authors’ own (adapted from Bastien-Olvera, Bernardo, and Moor 2021)
Digitalisation and interoperability
There has been increasing focus on digital solutions to achieve the goals of health and wellbeing. A major challenge regarding the use of multiple health systems by patients, care professionals, citizens, and institutions is the requirement of digitalisation and interoperability. Given public interest in the health sector, it is important to focus on open digital platforms such as Co-WIN (for COVID-19 vaccine registration) and contact-tracing (Aarogya Setu app), which have won global attention and praise (PTI 2023).
Another significant aspect is the need to ensure seamless portability of the health and wellbeing records of individuals for greater effectiveness in treatment and care to facilitate the location-agnostic treatment of people, including through access to telemedicine.
The increasing prevalence of digital health services, however, require as well as lead to substantial data collection, processing, storage, and transfer. Countries, therefore, have to formulate strong data-related policies and harmonise them with others where possible. Such a collaborative approach, which also incorporates an effective interoperability framework, can ensure that modern digitalised health and wellness systems promote access, equity, and inclusion.
The Global Digital Health Partnership (GDHP 2019)[c] describes ‘effective interoperability of information’ as the “key to attainment of the health-related Sustainable Development Goals (SDG) and to the improvement of the health and well-being of people across the world”. According to the GDHP (2019), such interoperability “provides the data resources for development of innovative mobile digital services and ‘apps’ that can support the patient, citizen and the care professionals who serve them”. Improvements in interoperability could enhance patient safety, coordination of care, and efficiency of healthcare delivery (GDHP 2019).
Interoperability here is a wider organising concept than the IT domain that it is most frequently used in. It describes the seamless exchange of data, information, physical structures, concepts, and contracts between socio-technical systems (Appelbaum 1997), making use of interoperability between involved stakeholders (Figure 2). Further, interoperability facilitates the reuse of existing resources and their integration into larger systems.
Figure 2: Extended Interoperability Conceptualisation for Global Socio-Technical System Success Improvement
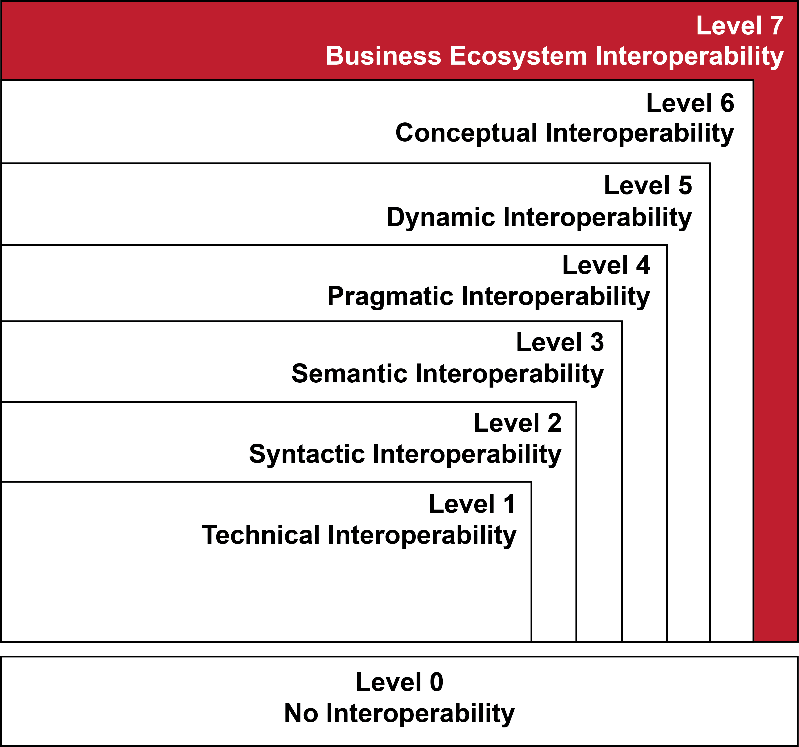
Source: Authors’ own (adapted from Tolk, Diallo, and Turnitsa (2007)
Sustained international regulatory dialogues are important to ensure that interoperability is among the good regulatory practices that promote openness. However, data anonymisation and security standards would be critical to build trust and acceptance of cross-national systems (Figure 3).
Figure 3: Interoperability of Health Systems and Wellbeing Systems Between Countries
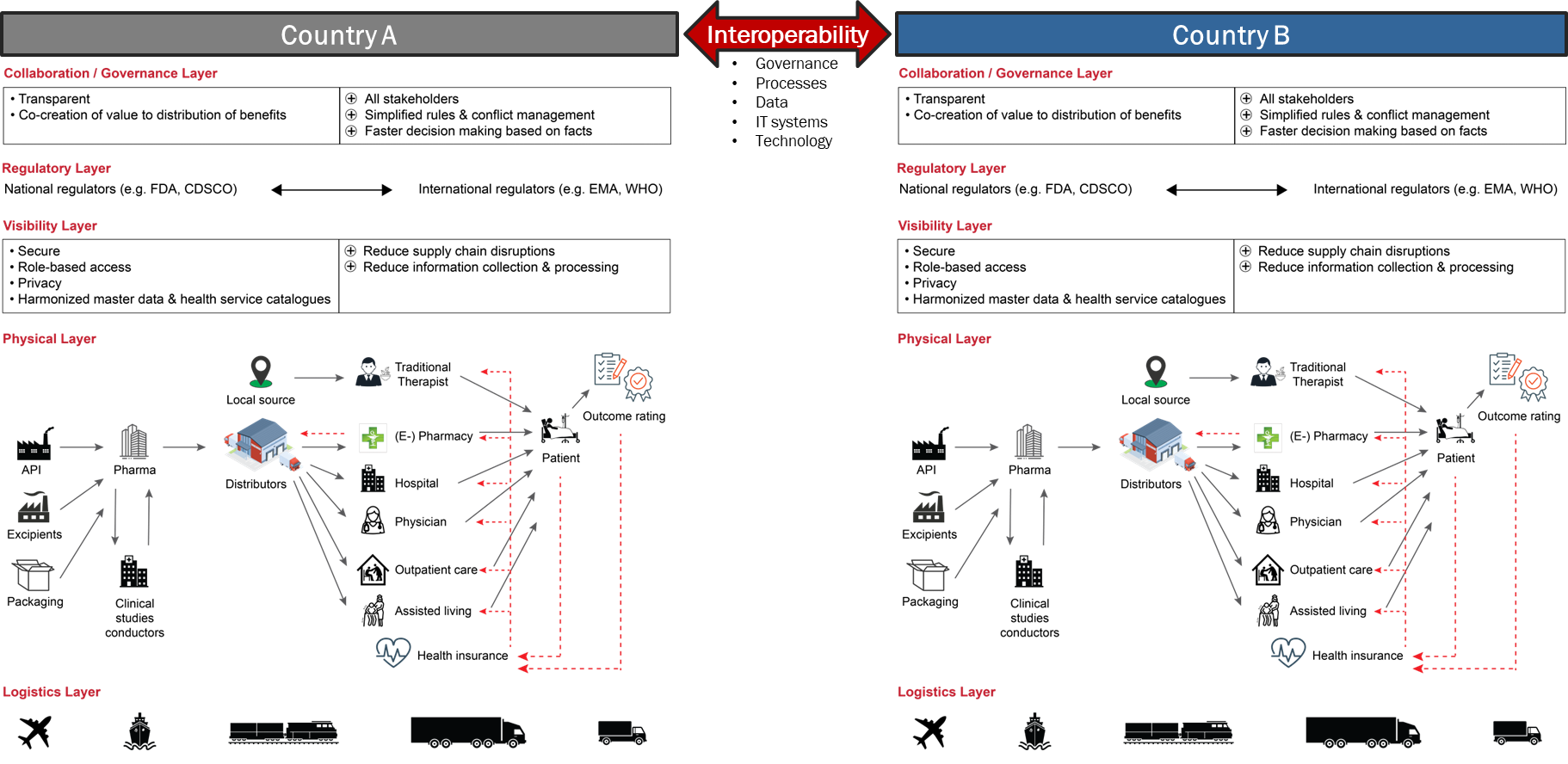
Source: Authors’ own
A case for global healthcare partnerships
Global collaborations and networks, as well as effective implementation of coordinated responses, have become unavoidable, given the increasingly cross-border nature of health risks in a globalised world as well as the financial constraints faced by most governments, especially those in the Global South (Gordon et al. 2022; Kher and Nair 2020).
These initiatives (Table 2) indicate that there is enough global appetite to forge multi-stakeholder partnerships to address various aspects of a people-centred approach to health and wellbeing. The goal of such global partnerships should be to expedite efforts towards achieving the objectives of the Tokyo Declaration on Universal Health Coverage (UHC).
They also make a case for reinforcing such efforts for a new global partnership by incorporating tools for digitalisation and interoperability, as well as a more open-minded but science-based approach to the regulation of various preventive, curative, and promotive healthcare approaches.
Table 2: Global Health Partnerships
| Partnerships | Area |
| · UN Central Emergency Response Fund
· The Global Fund · WHO Contingency Fund for Emergencies · World Bank Pandemic Emergency Financing Facility · Financial Intermediary Fund for Pandemic Prevention, Preparedness, and Response |
Large-scale mobilisation of finance for the health sector |
| One Health Global Leaders Group on Antimicrobial Resistance (AMR) | Ensuring that AMR is factored into health systems strengthening and health emergencies preparedness |
| Global Alliance for Ending AIDS in Children by 2030 | Child healthcare |
Source: Authors’ own (adapted from WHO 2022b; WHO 2020; UNCTAD 2022; WHO 2022d; WHO 2022c)
2. The G20’s Role
The G20 has taken note of the gaps in global pandemic preparedness and response and wants global health systems to have greater resilience, prevention, detection, preparedness, and response capacities (G20 Information Centre 2020). Recognising the vulnerability of health ecosystems to pandemics, the G20 has identified digital technology as an effective tool to pool expertise, utilities, and resources to overcome global health crises (G20 Information Centre 2020).
India’s G20 presidency’s first Health Working Group meeting discussed achieving holistic wellbeing through integrated healthcare (Government of India 2023c). Discussions also covered the need for equitable access to affordable and quality healthcare through a ‘One World, One Health’ approach, aligning with Vasudhaiva Kutumbakam (the world as one family) (Government of India 2023c). Prevention, preparedness, and response to health emergencies, digital health solutions helping with UHC and healthcare service delivery improvements, as well as ensuring access and affordability of vaccines, therapeutics, and diagnostics have been identified as the G20 priority areas in health (Government of India 2023d). The G20 will have to build on these proposals as well as existing global initiatives by facilitating the elimination of silo approaches and bringing the focus on links between wellbeing, the environment, and economic development.
3. Recommendations to the G20
This Brief proposes to enrich the One Health approach through a G20 Wellbeing Partnership incorporating a multi-disciplinary, multi-stakeholder, and human-centric strategy as an efficient and inclusive solution to address health-related challenges during pandemics and normal times.
The proposed partnership should be based on a strong foundation of trust, transparency, accountability, interoperability, and shared vision, in addition to access, equity, and inclusion (Schriger et al. 2021). For stronger and more effective partner involvement, it is crucial to help develop indigenous solutions as well as carry out monitoring, evaluation, and course corrections (Ramaswamy et al. 2016).
The main elements of the proposed partnership are given below.
a. Mainstreaming wellbeing
The interplay between wellbeing and economic growth/development has been affirmed by the WHO as a key component of the Geneva Charter for Well-being. The ‘mind-body-spirit’ component is increasingly recognised as vital to achieve the SDGs and objectives as envisaged in the Geneva Charter for Well-being (WHO 2021).
The G20 should identify actionable steps to mainstream this connect and recognise the role that it plays in the overall health of the individual. The G20 working groups on health, finance, development, digital, and trade and investment should consider including wellbeing and the proposed interconnected holistic interdependencies in their respective agendas.
b. Harmonising standards
Although it is a challenging task, harmonised certification and standardisation is critical to ensure healthcare quality. However, this needs to be done in a phased manner in developing economies, given their development challenges. The evolution of harmonised audit mechanisms for quality measurement, as well as voluntary accreditation systems and mandatory enforcement of standards, are required to promote quality and excellence. Further, setting minimum standards for healthcare entities and benchmarking national accreditation standards to international ones are crucial.
Setting, harmonising, and improving standards needs to occur on multiple levels:
- Professional education and training of standards (often national) as well as enforcement of standards directly by the government or through accredited third-party agencies
- Classification of diseases to be adopted further (e.g., the WHO’s International Classification of Diseases or ICD, which is used in 35 countries) (WHO 2022e)
- Data exchange standards (e.g., HL7 (Health Level 7), FHIR (Fast Healthcare Interoperability Resources)) to increase the use and interoperability of standards
c. Increasing interoperability
Interoperability is envisaged as a central element in the proposed partnership to strengthen the G20/global healthcare system framework and, in turn, help achieve the health-related SDGs and UHC.
The combination of building public-private business ecosystems or refocusing existing systems with the goal of outcome-focused measurement via interoperability-optimised organisations, processes, and IT systems (Figure 4) can help the G20 bring about a positive transformation in a central and entangled health and wellbeing SDG area, with positive spillovers in the natural, economic, and education system, among others.
Figure 4: Global Interoperability Framework for Socio-Technical Systems in Global Health and Wellbeing
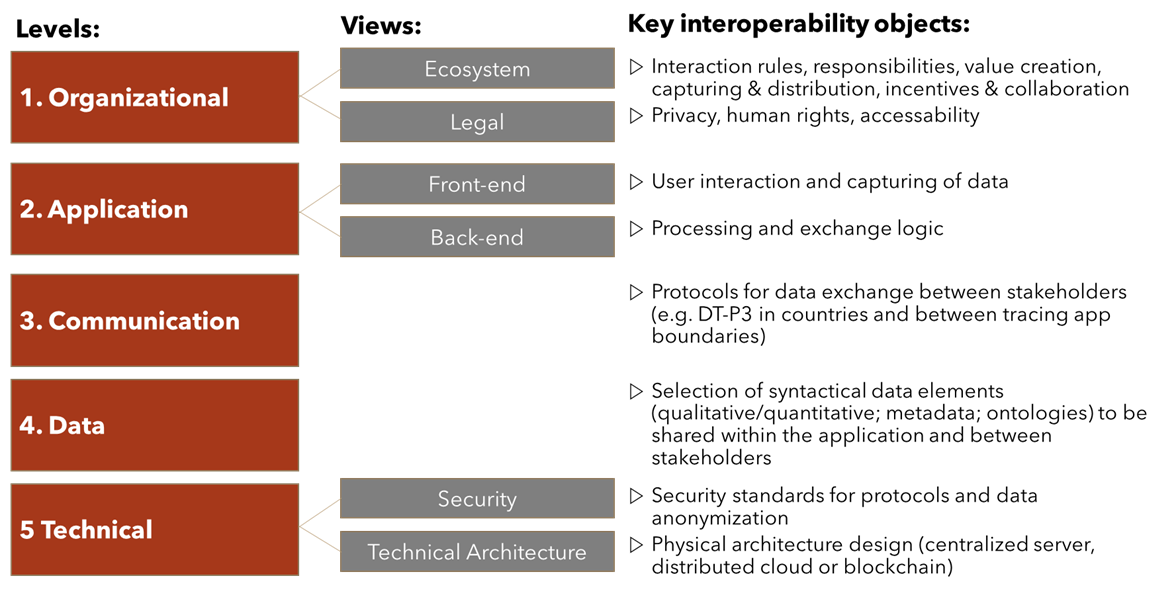
Source: Adapted from Nair and Klüber (2020)
Greater interoperability will benefit patients, service providers (through lower information costs and prices), and policymakers (through expeditiously addressing challenges such as pandemics or medical shortages). Efforts to extend the vision towards interoperable global health delivery systems need to overcome silo-thinking (e.g., national, geographical, modern medicine vs. traditional, IT literacy, data-sharing governance). Successful implementations need to build on five prerequisites towards improved wellbeing (Figure 5).
Figure 5: Prerequisites to Success
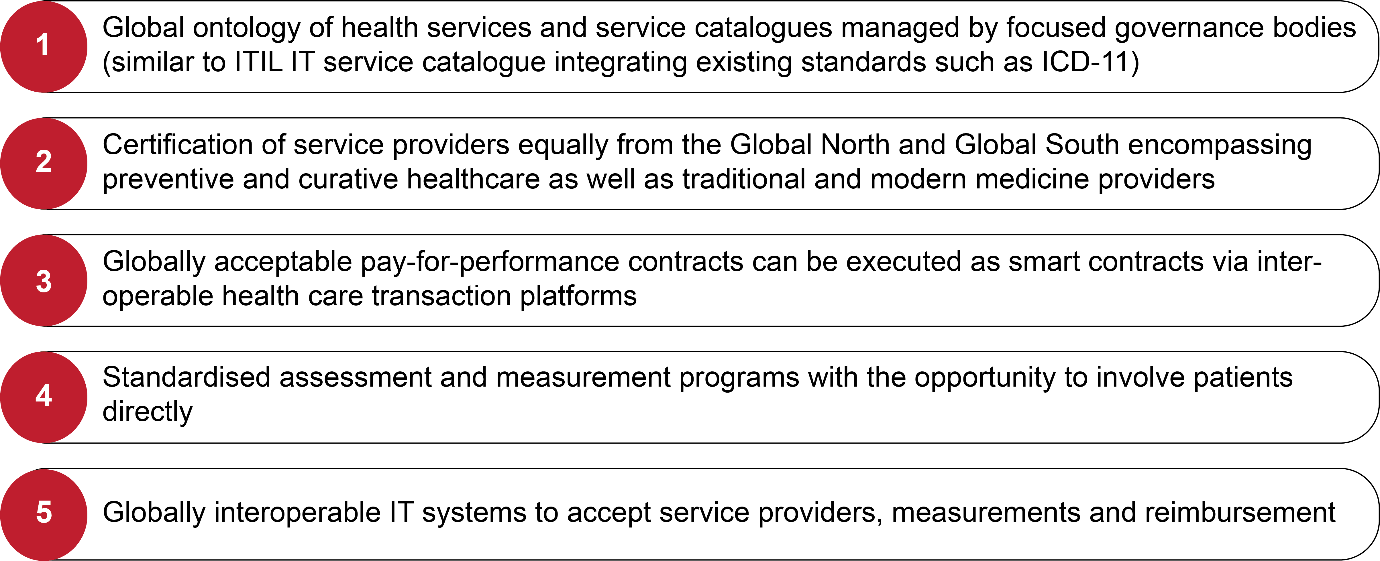
Source: Authors’ own[d]
The proposed success measures can help create a roadmap towards global interoperability of digitalised health systems that include privacy and data protecting cross-border portability of patient health files and health insurance, in addition to healthcare system interoperability at the organisational, national, and international regulatory levels. Given the data and security-related sensitivities, the mechanism moots a trustworthy public-private partnership model to initiate and scale up innovations enabling fast, efficient, and safe data exchange in global and trusted health ecosystems.
d. Enabling new opportunities within a more global health and wellbeing system
The G20 should mobilise support for the establishment of harmonised and interoperable measurement approaches by applying an outcome-focused system[e] to assess both traditional and modern medicine improvement therapies and preventive care treatments. This strategy will help link medical reimbursement systems to health insurance companies for regions and income groups where health insurance is available for all members of society. If complemented with anonymised access to patient data, the efficacy of an outcome-focused approach can be evaluated using modern (AI-based) IT systems. This can trigger a global learning process that helps identify the best treatment at the lowest cost for the identified diagnosis and towards optimised prevention or detection in the cure process. Profiling of customers and learning about successful (local) contexts and personal traits increases the success potential. As a consequence of reduced costs for health treatments and more efficient healthcare systems, health insurance can increasingly be made available in societies with a presently low coverage.
Patient-specific choice of treatments depends on the location and availability of medicines, modern medicine physicians and psychologists, or traditional therapists. Through the competition for the best-fitting health treatment, a global market is created for measurable health services towards their contribution to wellbeing. Tele-healthcare or tele-yoga are both possible but underused. Computer-mediated support can help match patients with the right service providers, including delivery and reimbursement. The outcome-focused approach can be efficiently expanded to traditional medicine across geographical dimensions by synergising existing global health partnerships and developing them towards interoperable socio-technical global health systems fostering wellbeing. A positive ‘by-effect’ would be the reduction of resource consumption and negative impacts on the natural systems, provided better health and wellbeing impact is achieved with lower costs and less CO2e impact.
4. Conclusion
The OECD 2021 drew on recent global experiences, with sound data-driven conclusions on the positive impact of wellbeing on the overall health of individuals in society. The G20 should holistically consider advancing global health system reforms, recognising the positive effects on wellbeing that are in harmony with the environment and other socio-technical systems.
Integrating traditional healthcare with modern medicine in an unbiased and comparable way, supported by standardised interoperable governance processes and IT systems, requires urgent commitment and investment. Such investments promise high commercial and social rate of return for the Global South and North. There is the need for a mindset shift such as that witnessed after the COVID-19 crisis, when global multilateral collaboration proved to be effective in confronting social challenges.
Attribution: Rajeev Kher et al., “Effective International Partnership for Health and Wellbeing: Interoperable, Holistic, Integrative,” T20 Policy Brief, July 2023.
Bibliography
Atluru, Aparna, and John Bracaglia. “An Outcomes-Focused Approach to Mental Health Care.” Harvard Business Review (March 2023). https://hbr.org/2023/03/an-outcomes-focused-approach-to-mental-health-care
Appelbaum, Steven. “Socio-Technical Systems Theory: An Intervention Strategy for Organizational Development.” Management Decision 35, no. 6 (1997): 452–63.
Bastien-Olvera, Bernardo A., and Frances C Moore. “Use and Non-Use Value of Nature and the Social Cost of Carbon.” Nature Sustainability 4, no. 2 (2021): 101–8. www.nature.com/natsustain.
Bhattacharya, Samir. “India’s Presidency Presents an Opportunity to foster India-Africa Collaboration on Traditional Medicines.” Vivekananda International Foundation, March 28. 2023. https://www.vifindia.org/article/2023/march/28/indias-g20-presidency-presents-an-opportunity-to-foster
G20 Information Centre. “G20 Health Ministers’ Declaration.” Last modified January 12, 2021. http://www.g20.utoronto.ca/2020/2020-g20-health-1119.html
G20. “G20 Bali Leaders’ Declaration”. November 15–16, 2022a. https://www.g20.org/content/dam/gtwenty/gtwenty_new/about_g20/previous-summit-documents/2022-bali/G20%20Bali%20Leaders%27%20Declaration,%2015-16%20November%202022.pdf
G20. “The Lombok G20 One Health Policy Brief.” 2022b. https://g7g20-documents.org/fileadmin/G7G20_documents/2022/G20/Indonesia/Sherpa-Track/Health%20Ministers/2%20Ministers%27%20Annex/The%20Lombok%20G20%20One%20Health%20Policy%20Brief_28102022.pdf
GDHP. “Connected Health: Empowering Health Through Interoperability. GDHP White Paper on Interoperability.” 2019. https://s3-ap-southeast-2.amazonaws.com/ehq-production-australia/57f9a51462d5e3f07569d55232fcc11290b99cd6/documents/attachments/000/102/278/original/GDHP_Interop_2.05.pdf
Gordon, Randolph., Alison Muckle Egizi, and John McInerny. “New Era of Global Public Health Partnerships: Collaborating for Better Health Preparedness.” Deloitte Insights, March 24, 2022. https://www2.deloitte.com/us/en/insights/industry/public-sector/government-trends/2022/global-health-partnerships-collaboration.html
Government of India. “G20 India Health Track. Ministry of Health and Family Welfare.” January 20, 2023a. https://pib.gov.in/PressReleasePage.aspx?PRID=1892409
Government of India. “G20 India Health Track. Ministry of Health and Family Welfare.” January 19, 2023b. https://pib.gov.in/PressReleasePage.aspx?PRID=1892239
Government of India. “G20 presidency’s first Health Working Group meeting held at Thiruvananthapuram.” PIB Delhi, January 20, 2023c. https://pib.gov.in/PressReleasePage.aspx?PRID=1892561
Government of India. “2nd G20 Health Working Group Meeting to Commence in Goa from 17 April.” Ministry of Health and Family Welfare, April 16, 2023d. https://pib.gov.in/PressReleasePage.aspx?PRID=1917099
Hein, Wolfgang. “Control of Communicable Diseases as a Global Public Good.” Med One 5, no. 1 (2020): 1-37. https://www.ssoar.info/ssoar/handle/document/69418.
Isidoro, Ciro, Chia-Chi Huang, and Lee-Yan Sheen. “Report from the Second International Conference of Traditional and Complementary Medicine on Health 2015.” Journal of Traditional and Complementary Medicine 6, no. 1 (2016): 5–9. https://www.sciencedirect.com/science/article/pii/S2225411016000031
James, T.C., Namrata Pathak, and Apurva Bhatnagar. “China’s Policy Initiatives for National and Global Promotion of TCM.” RIS. 2020. https://fitm.ris.org.in/en/node/994
Nair, Arun. S. and Roland Klüber. “Digital Contact Tracing Interoperability: Balancing Privacy and Public Health Concerns to Fight COVID-19.” Diplomatic Courier, September 25, 2020.
OECD. “Better Life Initiative: Measuring Well-Being and Progress.” Accessed March 19, 2023.
OECD. COVID-19 and Well-being: Life in the Pandemic. OECD Publishing, 2021. https://doi.org/10.1787/1e1ecb53-en.
PTI. “Bill Gates Praises India’s Progress in Different Sectors.” The Economic Times, March 4, 2023.
Rajeev, Kher, and A. S. Nair. “The Case for a Global Healthcare Partnership.” RIS Discussion Papers, 2020. https://www.ris.org.in/en/discussion-paper/global-healthcare-partnership.
Ramaswamy, Rohit, Brianne Kallam, Dragica Kopic, Borislava Pujic, and Medge D. Owen. “Global Health Partnerships: Building Multi-National Collaborations to Achieve Lasting Improvements in Maternal and Neonatal Health.” Globalization and Health 12, no. 1 (2016): 1–8. https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-016-0159-7
Schriger, Simone H., Agnes Binagwaho, Moses Keetile, Vanessa Kerry, Joel M. Mubiligi, Doreen Ramogola-Masire, Michelle Roland, Frances K. Barg, and Corrado Cancedda. “Hierarchy of Qualities in Global Health Partnerships: A Path Towards Equity and Sustainability.” BMJ Global Health 6, no. 12 (2021): e007132. https://gh.bmj.com/content/6/12/e007132.abstract
Tolk, Andreas, Saikou Y. Diallo, and Turnitsa. Charles D. “Applying the Levels of Conceptual Interoperability Model in Support of Integratability, Interoperability, and Composability for System-of-Systems Engineering.” Journal of Systems, Cybernetics, and Informatics 5, no. 5 (2007).
United Nations General Assembly (UNGA). “Resolution Adopted by the General Assembly on 19 July 2011.” United Nations, A/RES/65/309, August 25, 2011.
UNCTAD. “G20 Compendium on Promoting Investment for Sustainable Development (Bali Compendium)”. September 2022.
Uwishema, Olivier, Adekunbi Oluyemisi, Peñamante Criselle Angeline, Bekele Bezawit Kassahun, KhourCarlo y, Mhanna Melissa, Nicholas Aderinto, Adanur Irem, Dost Burhan, and Onyeaka Helen. “The Burden of Monkeypox Virus Amidst the Covid-19 Pandemic in Africa: A Double Battle for Africa.” Annals of Medicine and Surgery 80 (2022): 104197. https://www.sciencedirect.com/science/article/pii/S2049080122009578
WHO. “WHO Traditional Medicine Strategy: 2014-2023.” 2013. https://www.who.int/publications/i/item/9789241506096
WHO. “WHO Global Report on Traditional and Complementary Medicine 2019.” 2019. https://oialliance.org/wp-content/uploads/2019/06/WHO-GLOBAL-REPORT-ON-TRADITIONAL-AND-COMPLEMENTARY-MEDICINE-2019-2.pdf
WHO. “10th Global Conference on Health Promotion Charters a Path for Creating Well-Being.” March 4, 2021. https://cdn.who.int/media/docs/default-source/health-promotion/geneva-charter-4-march-2022.pdf?sfvrsn=f55dec7_21&download=true
WHO. “WHO Establishes the Global Centre for Traditional Medicine in India.” March 25, 2022a.
WHO. “New Fund for Pandemic Prevention, Preparedness and Response Formally Established.” September 9, 2022b.
WHO. “WHO Director-General’s Remarks at G20 Health Ministers Meeting – 20 June 2022.” 2022c. Accessed March 31, 2023.
WHO. “New Global Alliance Launched to End AIDS in Children by 2030.” August 2, 2022d.
WHO. “IDC-11 2022 Release.” February 11, 2022e.
WHO. “One Health.” Accessed February 20, 2023.
[a] In Africa, traditional medicine is culturally entrenched, accessible, and affordable and serves as a primary source of healthcare to more than 80 percent of the continent’s population (Isidoro et al. 2015). Holistic regimes such as yoga, a traditional Indian practice that promotes wellbeing through mental, physical, and nutritional practices, is widely recognised as an important instrument in ensuring wellbeing and health.
[b] Adapted from Bastien-Olvera, Bernardo, and Moor (2021). Some system design principles like gender equality need to be incorporated through the design, implementation, and success of measures intervening the often-isolated single system improvement approaches that undervalue interdependencies. The feedback mechanisms from the wellbeing status to the input and throughput elements are omitted for the benefit of a simpler graphical representation.
[c] The GDHP is a collaborative effort by governments, their agencies, and the WHO to ensure that digital health services are effectively implemented.
[d] Information Technology Infrastructure Library (ITIL) is a set of certifiable practices for IT services originating from the UK government initiative of the 1980s. The service catalogue comprises a curated and standardised set of IT services.
[e] The outcome-focused approach has been successfully applied to mental healthcare (e.g., Atluru and Bracaglia 2023).





