Taskforce 6: Accelerating SDGs: Exploring New Pathways to the 2030 Agenda- Promoting Holistic Outcomes in Health
Malaria continues to disproportionately impact vulnerable populations worldwide that are often located in rural and/or remote areas owing to weak health systems due to poor infrastructure, limited access to formal healthcare, and socioeconomic barriers. Malaria also robs countries of growth and development across all sectors and society, and imposes economic costs in the form of out-of-pocket and systematic healthcare expenditures. Additionally, some well-intended developments in other sectors such as agriculture, construction, energy, oil and gas, and mining may inadvertently fuel the spread of malaria. Countries are encouraged to develop innovative whole-of-government and whole-of-society approaches to respond to malaria in a coordinated and collaborative manner. National strategic plans for malaria elimination need to embed specific strategies that bring together all relevant health programmes as well as ministries, private sector, and other stakeholders to deliver services to these vulnerable communities and support malaria elimination.
1. The Challenge
With just seven years to achieve the targets of Sustainable Development Goals target 3.3 (communicable diseases[a]), including the goal to eliminate malaria, countries are being engaged to implement a ‘whole-of-government’ approach in the fight against this disease. As nations progress towards the elimination goal, malaria-endemic countries are facing challenges that requires them to move-away from ‘business as usual’ to address malaria through integrated policy and programmatic approaches across all sectors and stakeholders. This section lays out critical challenges that underpins the need for a ‘whole-of-government’ and ‘whole-of-society’ approach for malaria elimination.
Disproportionate malaria burden and risk of resurgence
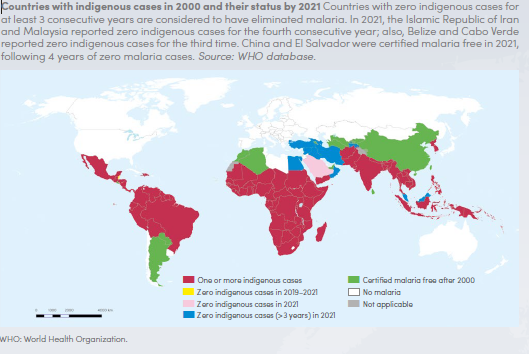
Over the last two decades, significant progress has been made in the fight against malaria. Globally, malaria incidence and mortality has declined by 28 percent and 51 percent, respectively.[1] Despite this, malaria is still endemic in 84 countries, disproportionately impacting vulnerable populations, people residing in rural, hard-to-reach and forested-fringed areas, and migrant communities along international borders. The influence of environment and society plays a big role in determining the health of the community, and the same holds true for malaria. At an individual level, household income, occupation, education, and gender are critical determinants that define the magnitude of exposure to malaria and access to health services.[2] Globally, 80 percent of malaria deaths are in under-five-children and pregnant women. In India, 30 percent of malaria cases and 40 percent of malaria deaths are reported from forested and ‘Adivasi’ districts, despite only accounting for about 7 percent of the total population. These geographies have environmentally favourable conditions for malaria transmission, coupled with weak health, water, and sanitation infrastructure, lower education levels and lower economic growth.[3] A study in Uganda showed that rural families spent up to 25 percent of their annual income seeking testing and treatment for malaria.[4]
Figure 1: Global Malaria Burden in 2021
Source: World Health Organisation: World Malaria Report – 2022
Population movement across borders, from malaria endemic areas to non-endemic areas and vice-versa, increases people’s exposure to malaria vectors, particularly in forest-fringe and border areas and high endemic neighbourhoods. The constant mobility increases the risk of malaria in both migrant and local populations, including the risk of resurgence.[5] While migrant populations and refugees are recognised as key vulnerable groups for malaria, the lack of full integration of their health needs into the host communities puts them at a higher risk, further derailing the progress towards sustained elimination.[6]
Economic impact across sector and society
Malaria takes an unnecessary toll on economic growth and development. Often referred to as a ‘disease of poverty’, the impact of malaria is manifold with consequences that go far beyond the impact on the health sector. Past studies have shown that malaria can reduce GDP growth by up to 1.3 percent.[7] It is estimated that the difference in economic growth rates between high malaria burden and malaria-free countries can be as high as six-fold.[8] In addition to the direct costs attributable to illness, diagnosis and treatment, and death, malaria also continues to contribute substantial societal costs. In endemic areas, malaria can significantly contribute to loss of workdays and schooldays, thereby having an impact on productivity, education outcomes, and economic growth.[9] In Africa, malaria is estimated to cause a combined loss of 584 million workdays each year, roughly the productivity of 2.4 million workers. In terms of fiscal impact, malaria is estimated to cost the African continent US$12 billion per year in lost productivity.[b] In India, the economic burden of malaria could be around US$1.9 billion, with major burden coming from lost earnings (75 percent) and the rest 25 percent from treatment costs.[10] The economic and development cost of malaria affects a broad swatch of sectors and industries, such as agriculture, mining, manufacturing, education, and tourism. Malaria endemic areas are estimated to receive 48 percent fewer tourists than those without malaria, resulting in approximately US$3.5 billion in lost tourism revenue globally each year.[11]
Cross-sectoral influence on malaria and need for integrated efforts
Competing health priorities and changing (both increasing and decreasing) malaria burden pose challenges to malaria-endemic countries. A decreasing burden poses the threat of a lack of commitment and deprioritisation of malaria efforts, particularly towards hard to reach last-mile interventions.[12] An increasing burden leads to a lack of confidence in existing interventions and reduced engagement by communities. Thus, there is a critical need to ensure that malaria elimination efforts are more holistic and cross-sectoral in nature. The need for integrated efforts and the role of other public and private entities and sectors is increasingly coming to light. For example, agricultural fields can potentially act as a breeding ground for malaria mosquitoes even though agricultural production is critical to food safety and economic growth, both in Asia and Africa. Similarly, migrant and mobile workers, pastoralists in malaria-endemic countries, working at construction sites, plantations fields, and the forestry industry, are at a higher risk of infection due to extended exposure to favourable conditions for malaria transmission. They also pose a great risk of resurgence due to constant mobility, especially in countries with shared land borders.[13]
Hence, it is essential to understand the intersectoral nature of malaria and the synergy between actions of various sectors to ensure the formulation of an informed and context-specific multisectoral and multistakeholder engagement. The actions taken by other sectors may have huge influence on malaria transmission. While the need for multisectoral/multistakeholder efforts for malaria elimination may be recognised, challenges are often faced in defining the roles and responsibilities of relevant sectors. This is due to the lack of understanding of the existing opportunities and benefits, both to health and non-health collaborating sectors.
2. The G20’s Role
Since its inception, the G20 has played a critical role in bringing together developing economies to collectively discuss economic and development issues, paving a way for concerted progress. As the foregoing narrative highlights, malaria directly affects “survival and the quality of life” and the ability of countries and individuals around the globe to achieve “just and equitable growth”. Ending malaria directly concerns several key priorities of the G20 which includes inclusive, equitable, and sustainable growth; LiFE (lifestyle for environment); women’s empowerment; digital public infrastructure and tech-enabled development in health, agriculture, education, commerce, skill-mapping, and culture and tourism; climate financing; circular economy; global food security; energy security; green hydrogen; disaster risk reduction and resilience; developmental cooperation; fight against economic crimes; and multilateral reforms. Only four of these priorities have limited or no link to the fight against malaria.
To illustrate this point, the G20’s first finance and health task force under Indian’s current presidency is a great example of a cross-sectoral initiative to strengthen global health architecture and disease response.[14]
Given this cross-cutting impact, engagement with heads of state and governments and ministers via the G20 presents an ideal opportunity to advocate for the adoption of a whole-of-government and whole-of-society approach for malaria elimination. It provides a critical forum that can be leveraged to directly engage with related sectors to advocate for inclusive and multisectoral dialogues, policy changes, sustained and increased financing, and well-coordinated action and resource mobilisation. The G20’s accountability mechanism (for instance, joint statements, accountability reports, and leaders’ declaration) can be leveraged to track progress and actions on the agreed multisectoral commitments, both nationally and internationally.
3. Recommendation to the G20
To address these challenges and strengthen the fight against malaria, the following recommendations can be considered to define the roles and responsibilities across sectors and advocate for the adoption of a whole-of-government and whole-of-society approach for malaria control and elimination.
Multisectoral coordination for malaria elimination
Cross-sectoral efforts requires malaria to be viewed through the lens of society, human and environmental behaviour, health equity, industrial growth, and sustainable economic development. Managing the environment, along with the impact of social norms and behaviours could considerably reduce malaria, however, these changes require a systemic approach to be driven by developmental and public policies, and governance systems.[15] Hence, extensive dialogues and evidence-based tools are necessary to identify opportunities and entry points for policy changes within each sector that can contribute towards the sector-specific goals and concurrently to malaria elimination efforts. Further, these cross-sector needs should be recognised in the national strategic plans for malaria to ensure an alignment of programmatic needs and proposed policy reforms. Examples from India, Zambia, Sub-Saharan Africa can be considered:
End Malaria Council, Zambia: The National Malaria Elimination Strategic Plan of Zambia (2022-2026) follows a multipronged approach that calls for a strong multisectoral collaboration—which includes public, private, non-governmental, faith-based organisations and academia—for successful malaria control and elimination.[16] Guided by the strategic plan, Zambia established the End Malaria Council (EMC) that includes the ministries of health, finance, tourism, and defence, the Bank of Zambia, the Zambia Revenue Authority (ZRA), several private sector companies, traditional leaders, and religious organisations. As a result of the collaboration through the EMC, ZRA identified trucks and other vehicles that could be used to distribute mosquito nets and other interventions and donated them to the National Malaria Elimination Centre. ZRA also donated television and radio advertising to promote social and behavioural change because of the adverse impact of malaria on the country’s tax revenues.[17] Likewise, the Ministry of Tourism has helped promote malaria messaging and installed collection boxes in national airports to mobilise funding from travellers. The Ministry of Youth and Sport has supported engagement with the Zambia Football Association, resulting in the recruitment of high-profile malaria champions from the national football team.[18]
One Health Consortium, India: India is leveraging the One Health approach to bolster cross-sectoral efforts with an aim to transition to a more integrated approach to zoonotic diseases. In 2021, the country’s first One Health consortium was launched to facilitate transdisciplinary research and multisectoral dialogues toward holistic approach to animal, human, and environment health.[19] Following this, through an undertaking by the Ministry of Fisheries, Animal Husbandry, and Dairying, the One Health framework pilot project was launched in Karnataka and Uttarakhand in 2022 to bring together animal, human, and environmental health stakeholders to develop a roadmap to prevent future zoonotic diseases, such as bird flu and rabies, equipped with better response mechanisms and management.[20]
New Nets Project and Nets Transition Initiative, Sub-Saharan Africa: To help address the growing threat of insecticide resistance in the fight against malaria, in 2018 the Global Fund and Unitaid, working closely with countries in Sub-Saharan Africa (Benin, Burkina Faso, Burundi, Cameroun, Cote d’Ivoire, Democratic Republic of Congo, Ghana, Guinea, Liberia, Mali, Mozambique, Niger, Nigeria, Senegal, Sierra Leone, and Uganda) and key malaria partners, launched a catalytic investment to help accelerate the scale up of dual active ingredient nets. The New Nets Project and Nets Transition Initiative supported countries to generate the strong evidence needed on the impact of pyrethroid-chlorfenapyr dual active ingredient nets, as well as increasing the supply capacity of manufacturers, and stimulating price reductions through economies of scale.[21] As a result of this work, countries have developed capacity, reflective of local needs, to implement mixed net campaigns, and the production capacity for these nets has increased. In 2023, the World Health Organization issued a strong recommendation on the use of the pyrethroid-chlorfenapyr nets. This has added an extremely impactful vector control intervention to the malaria toolbox.[22]
Malaria-inclusive policies
Underpinned by the concept of ‘Health in All Policies’, the whole-of government and whole-of-society approach for malaria elimination calls for policies across sectors to systematically take into account the implications of their policy decisions on malaria transmission, recognise the existing synergies, and shared accountability of a malaria-free population.[23] It requires the sectors to proactively include prevention, surveillance, vector management, and diagnosis and treatment as part of their sectoral plans in a cost-effective and integrated manner. Examples from following sectors could be considered:
Agriculture: Food production practices may create favourable conditions for the breeding of malaria vectors; irrigation reservoirs, water storage systems/and broken water pipes, deforestation, and land use may affect humidity, temperature, and vegetation, leading to changes in local ecology, which can in turn impact vector behaviour and growth. In addition, the use of herbicides and pesticides may affect insecticide resistance—a major challenge in malaria-endemic countries.[24] In turn, malaria may adversely affect farmers, both in terms of health and agricultural productivity. Hence, malaria inclusive policies need to be considered within the agriculture sector to negate the impact on malaria transmission, at the same time improving food production and farmers’ health. For example, the Khartoum Malaria-Free Initiative in Sudan was launched with stakeholders (such as those from health, agriculture, education, and public works) closely involved at the state and federal levels to address the fact that the expansion of agriculture and construction sites and failure to fix broken water pipes were supporting to create mosquito breeding habitats in Khartoum.[25]
Energy and Mining: The increased need for energy and natural resources results in greater deforestation, environmental altercations, and the influx of migrant population associated with such projects, which can in turn influence malaria transmission, resulting in increased disease incidence. Malaria cases attributed to hydroelectric projects were found in Asia[26] and Africa[27] with the majority of the burden in those living in close proximity of the dam area. Similarly, rainwater in mining pits can create breeding sites for malaria mosquitoes.
In Brazil, a jointly developed regulation for cross-sectoral collaboration, involving the ministries of health, environment, and mines and energy, and the National Foundation of Indigenous People, was developed to reduce the direct and in-direct impact of infrastructure and extraction projects in malaria-endemic areas. It required companies to conduct assessment, recommend actions, and allocate funds to support malaria control before obtaining license to operate in the area.[28]
In Mozambique, the Fundo da Malaria and Goodbye Malaria programmes have engaged several energy and oil and gas companies to mobilise resources for vulnerable populations. These companies have pledged millions of dollars to support malaria interventions in rural communities.[29] And there is growing interest in seeing how investments made by large multinational companies to develop the Rovuma Basin off the coast of Cabo Delgado (an area with amongst the highest concentration of malaria globally) can support malaria control for at-risk populations.[30]
Education: Education is one of the key socioeconomic determinants of health. There is a clear link between education level and malaria related morbidity and mortality. Low education level substantially adds to the compounded effect of socioeconomic risk factors and increases people’s susceptibility to exposure to malaria vector. Several studies have reported the negative co-relation between maternal education and risk of malaria in children. It impacts the health seeking behaviour and child’s access to malaria prevention and treatment.[31] Malaria is also associated with poor education outcomes in school children, including loss of school days and educational performance.[32] In Uganda, Malaria smart school programmes are being piloted to incorporate malaria education into the school curriculum. Under this programme, the school students are provided comprehensive knowledge of malaria with a primary aim to break the community behavioural cycle through learning.[33]
Attribution: Shubhla Singh et al., “Developing a Whole-of-Government, Whole-of-Society Approach for Malaria Elimination,” T20 Policy Brief, July 2023.
[a] Target 3.3 focusses on ending the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases, and combating hepatitis, water-borne diseases, and other communicable diseases.
[b] Analysis by the African Leaders Malaria Alliance using regional benchmarks on worker absenteeism
[1] World Health Organization, World Malaria Report 2022, Geneva, WHO, 2022.
[2] Indumathi Mohan et al., “Socio-economic and household determinants of malaria in adults aged 45 and above: analysis of longitudinal ageing survey in India”, Malaria Journal (2021): 20, 306.
[3] Raju Ranjha and Amit Sharma, “Forest malaria: the prevailing obstacle for malaria control and elimination in India”, BMJ Global Health (May 2021), 6-5.
[4] National Malaria Control Division, Ministry of Health of Uganda, Malaria Programme Review (2017)
[5] World Health Organization, “Approaches for mobile and migrant populations in the context of malaria multidrug resistance and malaria elimination in the Greater Mekong Subregion”, New Delhi, WHO, 2016.
[6] World Health Organization, “Population mobility and malaria”, New Delhi, WHO, 2017.
[7] Monica V. Andrade, “The Economic Burden of Malaria: A Systematic Review”, Malaria Journal, no. 21 (2022): 283.
[8] Jeffrey Sachs and Priya Malaney, “The economic and social burden of malaria”, Nature, 415 (2002):680–685.
[9] Seun Anjorin, Elvis Okolie, and Sanni Yaya, “Malaria profile and socioeconomic predictors among under-five children: an analysis of 11 sub-Saharan African countries”, Malaria Journal 22 (2023): 55.
[10] Indrani Gupta and Samik Chowdhury, “Economic burden of malaria in India: The need for effective spending”, Journal of Public Health, (January – March 2014):95-102.
[11] Jaume Rosselló, Maria Santana-Gallego, and Waqas Awan, “Infectious disease risk and international tourism demand”, Health Policy and Planning, vol 32, No. 4 (May 2017): 538-548.
[12] “Polio eradication: falling at the final hurdle?”, The Lancet, volume 400, issue 10358, (2022): 1079.
[13] World Health Organisation, “An Urgent Front: Cross-border Collaboration to Secure a Malaria-free South-East Asia Region”, New Delhi, WHO, 2018.
[14] “1st Joint Finance and Health Task Force Meeting”, G20, accessed March 13, 2023.
[15] Roll Back malaria and United Nations Development Programme, “Multisectoral Action Framework for Malaria“, Geneva, Roll Back Malaria and UNDP, 2013.
[16] Ministry of Health, Republic of Zambia, National Malaria Elimination Strategic Plan, 2017.
[17] “End Malaria Councils & Funds: Introduction”, ALMA Scorecard Hub, accessed March 15, 2023.
[18] “End Malaria Council Meeting“, Zambia National Malaria Elimination Center, accessed March 15, 2023.
[19] Department of Biotechnology , Ministry of Science & Technology, Government of India, “Country’s First ‘One Health’ Consortium Launched by D/O Biotechnology, Post COVID 19,” October 14, 2021,
[20] Ministry of Fisheries, Animal Husbandry & Dairying, Government of India.
[21] “Results Report 2022”, The Global Fund, accessed May 29, 2023.
[22] World Health Organisation, “WHO guidelines for Malaria, 2023”, Geneva, WHO, 2023.
[23] World Health Organisation, “Intersectoral Governance for Health in All Policies“, Copenhagen, WHO, 2012.
[24] Sara A. Abuelmaali et al., “Correction: Impacts of Agricultural Practices on Insecticide Resistance in the Malaria Vector Anopheles arabiensis in Khartoum State, Sudan”, PLoS ONE; no. 8:12 (2013).
[25] Roll Back Malaria and UNDP, “Multisectoral Action Framework for Malaria”
[26] Shiva Raj Mishra et al., “Threats to Malaria Elimination in the Himalayas“, The Lancet, (2016):8.
[27] Lili R. Mbakop et al., “Malaria Transmission around the Memve’ele Hydroelectric Dam in South Cameroon: A Combined Retrospective and Prospective Study, 2000-2016”, International Journal of Environmental Research and Public Health; 16(9): (May 9, 2019): 1618.
[28] Roll Back Malaria and UNDP, “Multisectoral Action Framework for Malaria”
[29] “End Malaria Councils & Funds Webinar (13 July 2021)”, ALMA Scorecard Hub, accessed March 15, 2023.
[30] “Preventing Malaria Among Internally Displaced Persons in Mozambique”, US President’s Malaria Initiative, accessed March 16, 2023.
[31] “Fact Sheets on Malaria and the SDGs – Education and malaria“, Partnership to End Malaria, accessed March 16, 2023.
[32] Erin M. Milner et al., “Association between Malaria Infection and Early Childhood Development Mediated by Anemia in Rural Kenya”, International Journal of Environmental Research and Public Health. 2;17(3)(2020 Feb): 902.
[33] “Expanding “Malaria Smart Schools” in Uganda Will Help End Malaria”, Malaria Matters, accessed March 16, 2023.