TF-6: Accelerating SDGs: Exploring New Pathways to the 2030 Agenda
Non-communicable diseases (NCDs) are the largest cause of mortality and premature deaths worldwide, killing 50 million people every year.[1] NCDs can be controlled through awareness and preventative and curative interventions. Yet, there is no global solution that can identify individuals at risk and enable the effective and equitable scaling of evidenced treatments. This brief proposes policy actions for the G20 to facilitate the creation and adoption of a digital public health system for NCDs and proposes an open-source model that includes artificial intelligence-based screening, behavioural-change strategies, and evidenced preventative and curative treatment modalities. The policy brief discusses the potential of such a system in helping achieve target 3.4 of the Sustainable Development Goals of reducing premature mortality from NCDs by one-third through prevention, treatment, and the promotion of mental health and well-being by 2030. Such a digital health system could also be a step towards the global goal of universal health coverage.
1. The Challenge
Non-communicable diseases (NCDs) are chronic diseases that are not caused by infectious agents and progress slowly over a long duration of time. Examples include, heart disease, stroke, obesity, mental health issues, diabetes, and chronic respiratory diseases.[2]
These diseases contribute to around 71 percent of all deaths worldwide, with 14 million premature deaths occurring between ages 30 and 70.[3] Low-and-middle-income countries (LMIC) bear 86 percent of these premature deaths, causing a US$7 trillion economic loss, trapping millions in poverty.[4] Most of these premature deaths are preventable by enabling health systems that can screen, predict, and treat NCDs utilising early interventions.
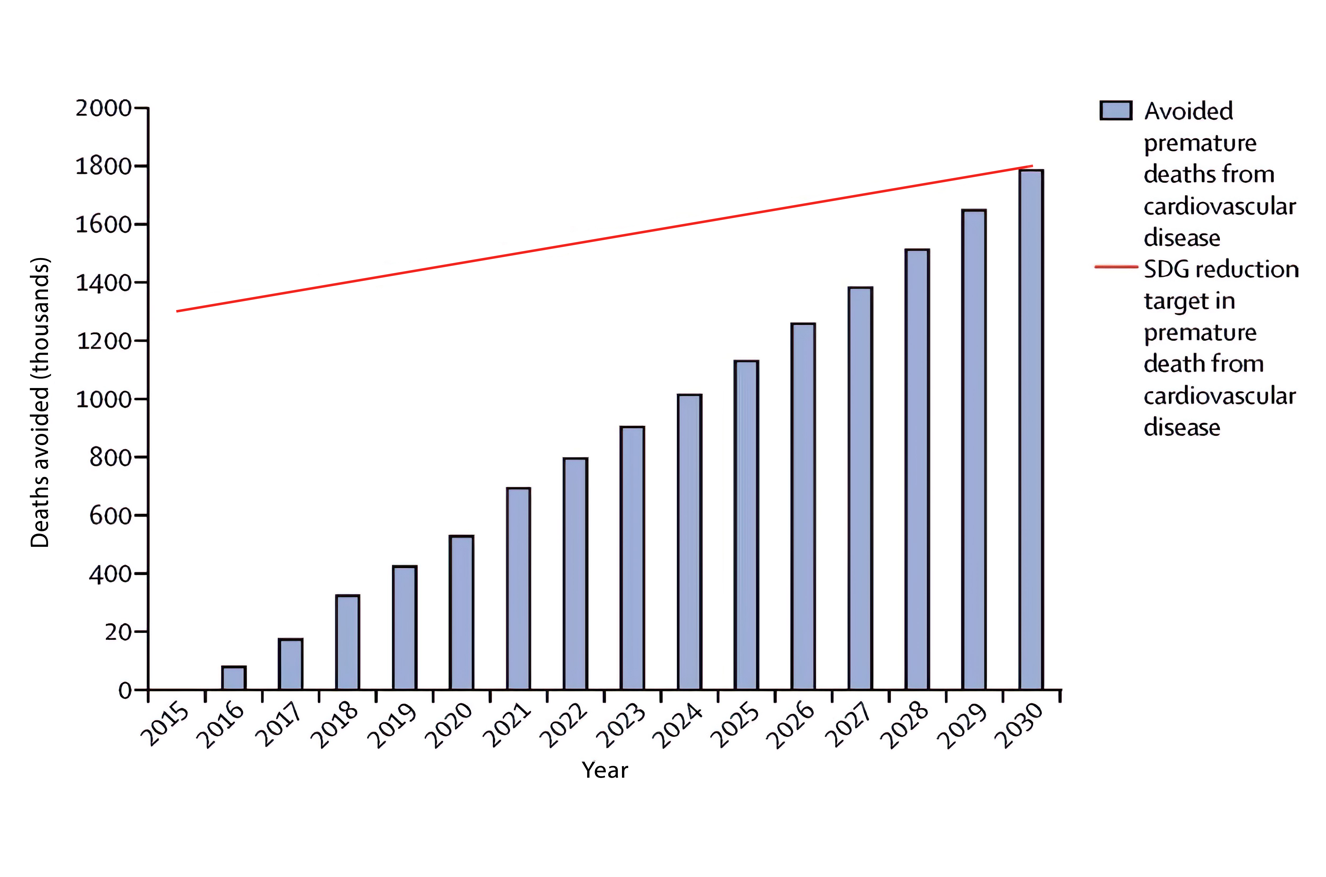
Figure 1: Global trends in non-communicable disease mortality and progress towards SDGs target 3.4

Source: Bennet et al.[5]
There is a clear need for a digital global health system that can responsibly screen people for NCDs, and map them accurately with the appropriate evidence-based interventions for prevention and control.
Furthermore, such a system could potentially be used to track the effectiveness of various preventative measures and treatments for NCDs, providing valuable insights into which interventions are most successful in tackling these diseases.
Therefore, a globally scalable ABC (Assessment, Behaviour change, and Care management) system is essential for addressing NCDs and realising SDG 3.4.
2. The G20’s Role
NCDs are one of the biggest population health risks in low-to-middle income countries.[7] In recognition of the need, World Health Organization’s Department of Noncommunicable Diseases launched the Global NCD Compact 2020–2030, urging member states to adopt best-practice policies for NCD prevention and control. The initiative aims to scale existing preventative care and treatments available, reduce NCD burden by one-third, and save 50 million lives by 2030.[8]
Since the Berlin Summit in 2017, the G20 has strongly focussed on working together to promote, provide, and support global health and well-being standards and collaborating to achieve universal health coverage. There have been active deliberations and specific recommendations to develop and scale digital health solutions (in Berlin 2017, Buenos-Aires 2018, and onwards) to tackle some of the largest health challenges that the world faces today. These digital health interventions focus on many areas including, but not limited to, responsible data sharing for early identification of health risks, adopting best practices for health, and scaling best treatment practices to enable equity, affordability, and high-quality outcomes globally.
The G20, representing technologically advanced and advancing nations, can, therefore, support the efforts of The Global NCD Compact 2020-2030, by creating policies, solutions, and directives for NCD management.
Investing in NCD prevention and control is attractive, as cost-effective, high-impact interventions already exist, but due to lack of early detection and difficulty in scaling these interventions, high mortality, and NCD-related health burdens continue to exist. The WHO estimates that close to seven million lives can be saved by 2030 with an additional investment of US$0.84 per-person/year in LMICs. Furthermore, health gains, when converted into economic and social benefits, are estimated to be worth more than US$ 230 billion.[9]
The G20 nations can contribute to developing a preventative screening mechanism to identify high-risk communities, individuals, and regions, and map them with evidence-based existing and emerging interventions.
Figure 2: Estimated return on investment for prevention and treatment services
Source: Bertram et al.[10]
3. Recommendations to the G20
This section presents the proposed framework for the development of an NCD response digital screening, prevention, and behavioural-health system. The system is developed on behaviour change principles and brings ABC for NCDs together on a common digital platform, bridging the gap in the availability of treatments and raising awareness across countries.
ABC digital public health infrastructure model
A for ‘Assessment’: Implement evidence- and score-based classification along with an Artificial Intelligence (AI)-led predictive screening tool that accurately analyses NCD risk factors, current health status, and lifestyle choices.
B for ‘Behaviour change’ strategies: Bring about behaviour change in target populations, encouraging a healthier lifestyle, awareness, and a preventive mindset regarding NCDs.
C for ‘Care management’: Offer health programs on all existing digital-health-systems. These programs should include digital-therapeutics and lifestyle tracking. Additionally, they should contain tools for patients, as well as digital training and detailed protocols for healthcare/frontline workers for management of NCDs. This system will enable efficient and effective scaling up of already present interventions that are both preventive and curative.
Also, the open digital health system aims to facilitate the global dissemination of evidenced lifestyle management sciences and practices. It also seeks to support new intervention development, research and innovation by academia, and facilitation of the start-ups and health-ecosystem.
Figure 3: ABC model of open digital public health infrastructure
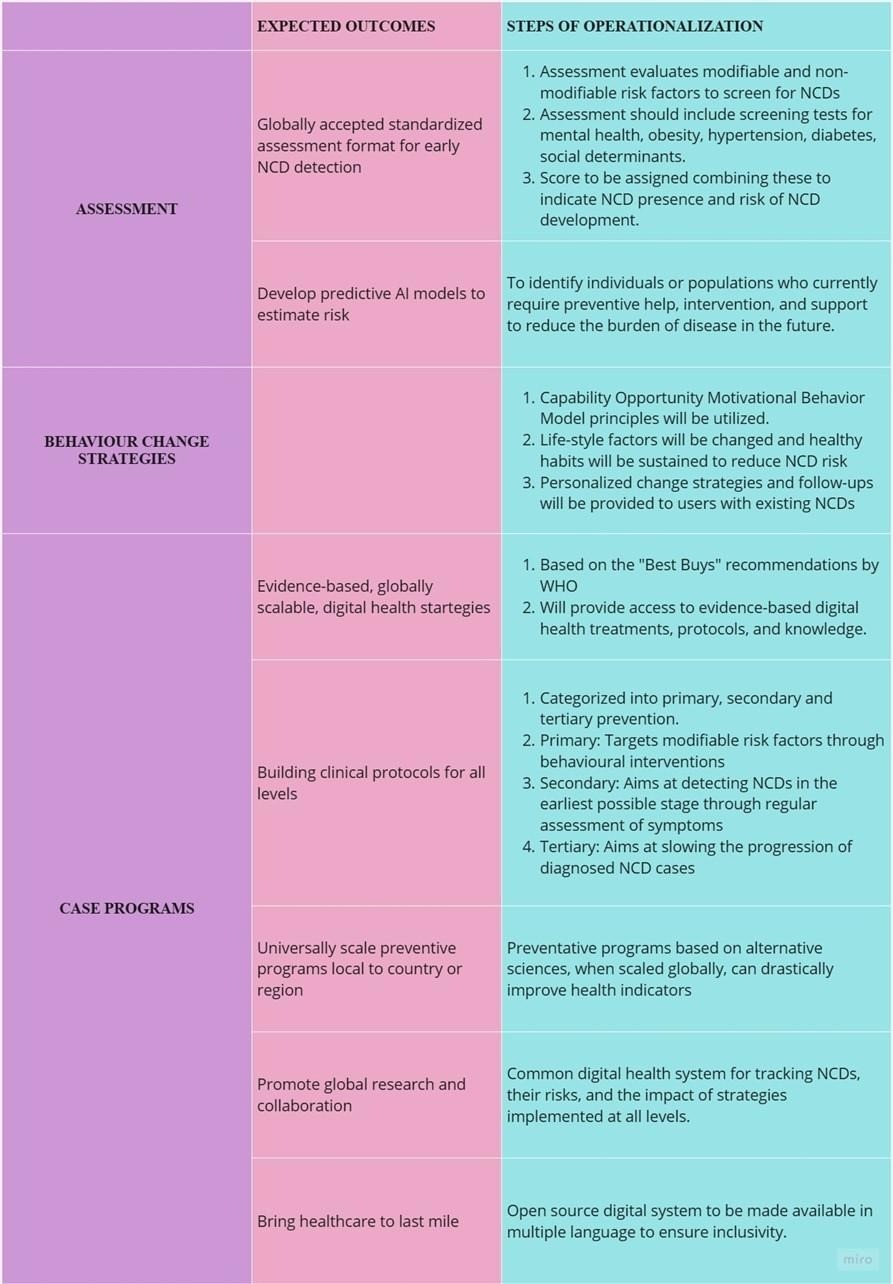
Assessment
a) Create a standardised assessment format that is globally accepted for early detection of NCDs
To effectively screen for NCDs, it is recommended that the G20 nations develop a standardised assessment that evaluates the user’s risk factors for prevalent NCDs. This assessment should be organised into two key sections: modifiable and non-modifiable risk factors.[11]
The section on non-modifiable risk factors should encompass questions regarding age, gender, family history, and ethnicity. Based on the answers provided, a list of the most common NCDs that may arise with those specific demographic features can be generated. The subsequent section on modifiable risk factors, should address the user’s habits such as smoking, drinking, physical activity, weight, and diet. By delving into these details, a more refined list of probable NCDs that may occur in the individual can be created. Further questions may be asked based on this narrowed-down list, specifically pertaining to the earliest symptoms associated with each NCD to better predict the risk of each one.
This screening test can include questions on mental health, reproductive health, obesity, hypertension, and diabetes as a starting point. Screening for social determinants (e.g., income, education, and environment) and associated risks that could contribute to developing NCDs in the future could also be included.
The screening system will have one single score combining many factors. By using this approach, a more comprehensive and tailored risk assessment can be conducted to facilitate early detection and management of NCDs.
A similar concept in the form of a ‘Digital Health Scorecard’ has been proposed by an American study. In this, the overall health score is calculated on a scale of 0 to 100, with 100 being the ideal score. The application uses a simple formula with 2 variables that are dependent on user input. However, this system did not take into account family histories, diet, emotional health, and immunisations.[12]
b) Developing predictive models using AI to discern global growth and incidence of NCDs
Predictive AI models can be developed by analysing data on the current patterns of disease incidence at regional, national, and global levels. These models will capture social determinants and risk factors and accurately predict the incidence and burden of disease. They can identify populations that require preventative help and support. Acting on these predictions can dramatically reduce future disease incidence and burden.
Behavioural change
Embedding principles of the Capability-Opportunity-Motivational Behaviour Model, the digital health system can help those identified with a high risk of developing NCDs with behavioural tools to effectively change their lifestyle, sustain habits that reduce the risk of developing NCDs, and promote health and well-being. Further, those identified with NCDs can be helped through personalised change strategies to adhere to mapped treatment. In addition, they can be encouraged to participate in ongoing follow-ups to assess their health status and continue treading the path to recovery and good health. Behavioural change strategies have shown strong evidence of helping individuals adopt healthier lifestyles and adhere to the recommended management programs.
An analysis of over 50 studies on the usage of behavioural digital health interventions for NCD management found that behavioural interventions had an overall positive effect. Specifically, digital availability of these interventions has demonstrated a positive influence on self-management activities and encouraged healthy lifestyle choices, including improved adherence to medications, awareness, and increased physical activity.[13]
Figure 4: The effectiveness of digital health for non-communicable disease management in primary health care in included trials

Source: Xiong et al.[14]
a) Evidence based digital health strategies that can scale globally
On the basis of the scorecard and any personalised need of intervention, individuals and healthcare providers and entities, can be provided access to evidence based digital health treatments, protocols, and knowledge. This will allow for faster scaling of both curative and preventative solutions in a cost-effective way.
The WHO’s ‘Best Buys’ report is a list of the most cost-effective and high-impact interventions that can be implemented to address NCDs such as cardiovascular disease, cancer, diabetes, and chronic respiratory disease. The document provides a framework for planning and implementing interventions based on their affordability, cost-effectiveness, and potential to reduce the burden of NCDs.[15]
Here are a few examples of how the Best Buys recommendations can be integrated into the proposed system:
- Offer mobile phone-based tobacco cessation services to users who have a habit of smoking.
- Provide concise psychosocial interventions for users who report harmful alcohol use.
- Incorporate physical activity and counselling into treatment plans using an interventional approach.
- Deliver preventive foot care to individuals with diabetes, which includes educational content on foot care and reminders for self-examination.
- Consistently provide reminders to ensure that individuals receive tests like mammograms and other check-ups based on their age group and existing conditions.
b) Building clinical protocols for all levels
To effectively prevent NCDs, it is recommended to adopt a multi-level approach comprising primary, secondary, and tertiary-level preventions.
Primary prevention aims to reduce risk factors, typically by implementing behavioural interventions to target modifiable risk factors. For instance, self-monitoring, goal setting, and lifestyle changes can be introduced to the user in a digital, gamified format.
Secondary prevention aims to detect NCDs at their earliest stages. Regular user input on relevant signs and symptoms, preferably on a weekly or monthly basis depending on the symptom, can be collected and compared to the baseline level established at registration. Any significant deviations from the baseline can trigger an alarm, prompting the user/healthcare provider through the system.
Tertiary prevention aims to manage NCDs after diagnosis. This stage typically involves complex clinical protocols that are specific to each disease and its stage of diagnosis. Evidence-based lifestyle changes can be introduced as behavioural interventions in a gamified manner, similar to primary prevention. Tertiary prevention can also involve medication reminder systems and adherence monitoring systems.
By adopting this multi-level approach, a comprehensive and tailored strategy for preventing, detecting, and managing NCDs can be developed, ultimately leading to better health outcomes for individuals.
This concept has, to an extent, been explored by a study in England, which found that a simple web-based, self-management intervention significantly lowered glycated haemoglobin (HbA1c) levels in patients in a span of 12 months.[16]
c) Scaling local preventative programs globally
Preventative programmes like yoga from India, Qigong from China can be made available and scaled globally for specific NCD management. For example, digital yoga programs can be created and adopted universally for specific issues like obesity, cardiovascular wellness, and general well-being. These specific intervention-based digital programs can further be studied for their impact and efficacy at a global level. When scaled internationally, these alternative and highly effective sciences and behavioural practices can drastically improve health indicators.
d) Promoting research and collaboration amongst academicians, innovators, healthcare practitioners, and global organisations
The implementation of a unified digital-health system to monitor NCDs and their associated risks, along with the adoption of evidence-based strategies for managing NCDs, could lead to the creation of new research and development initiatives. It could further prompt coordinated population health management systems and protocols at the regional, national, and global levels. This digital-health system will allow registration, active participation, and collaboration to achieve the global SDG of health and well-being.
e) Frugal and evidenced innovation to bring healthcare underserved communities
This open-source digital screening, management and prevention system should be made available in multiple languages and should provide evidenced care digitally at reduced costs. Digital system should also enable accessibility to underserved areas and thus contribute to universal health coverage.
Including other NCDs
The first phase can focus on NCDs such as mental health, diabetes, reproductive health, and hypertension. After successful implementation and impact assessment of the digital health system in reducing the burden of select NCDs, other NCDs can be included in a phased manner.
Specific policy recommendations to the G20
- Create a sub-task force charged with the creation of a digital evidenced health system for NCDs under the Joint Health and Finance Minster’s Task Force that collaborates with IT/technology, healthcare research organisations, global technology companies, digital systems and security, and welfare organisations across the G20. This task force will further be entrusted with developing, testing, deploying and assessing the impact of this global digital health system.
Policy actions: Deliberate and establish commitment under the aegis of the ‘global initiative on digital health’, announced in June 2023, for the development of the digital health system proposed for NCD management.
Establish a framework to ensure maximum participation of all G20 nations and enable leadership structures.
Address issues with the process of identifying people with existing or high risk of NCDs through the creation of a digital screening system based on a health score card that can effectively assess and identify risk of NCDs for individuals across G20 nations.
Policy actions: Ensure the development of a health score card that is common and universal. This would require reviewing existing evidence-based healthcare score cards, and selecting the most effective, accurate, and scalable ones that can test the presence of NCDs through a digital system which is accessible to all G20 nations. This needs to be supported and scaled through a corroborative policy direction.
Enable a framework to help nations with similar screening systems to adopt the common healthcare scorecard and incentivise sharing best practices.
- Encourage countries and healthcare organisations to share evidence-based interventions and best buys to include in the digital health system that can be scaled to all nations. Creating a nationally favourable regulatory environment for the development of best buys that can help prevent and control NCDs.
Policy actions: Establish an internationally accepted toolkit and framework, supported by regulatory guidelines, for evaluating, selecting, and making available best buys, that are evidenced by digital therapeutics or protocols for controlling and preventing NCDs through a digital system.
Expand efforts to provide sustainable financing to start-ups, researchers, healthcare individuals, and institutions for developing evidence-based preventive and curative digital care models for further control of NCDs.
- Address country and region specific NCD treatment and prevention gaps by developing a digital system in select nations in the first phase and up-skilling healthcare workers and human capital in this identified group for executing successful scaling up.
Policy actions: Mapping and tracking nations with the most gaps for NCD treatment adoption as well as good readiness to be included in the first phase of scale up.
Set up mapping, tracking, and anticipation systems to incorporate digital skills into the up/re-skilling initiatives of healthcare workers, while developing standard operating procedures to initiate the roll out of a global digital health system.
- Analyse gaps in digital maturity across G20 nations and scale the digital infrastructures nations lagging behind, utilising the expertise of nations that have developed efficient public digital health goods and frameworks.
Policy actions: The G20 should identify countries working in the global Digital Public Health Infrastructure (DPHI) development space and appoint a nodal body that can help accelerate and enhance the digital maturity of nations, leveraging existing DPHI and knowledge.
The G20 should promote multi-stakeholder collaboration across nations for the development of further open-source models that allow responsible global scaling-up, cost savings, innovation, and building trust in the system to foster cross-border interoperability.
- Promote cross-national research to develop more evidence-based solutions and help scale these across G20 nations. The forum should further encourage a culture of innovation and invention in G20 nations by promoting start-ups and academic projects that deal with the prevention and control of NCDs.
Policy actions: The G20 should develop an accepted framework to help promote research, responsible data sharing, and cyber security best practices that are consistent and interoperable across regions.
The G20 should further develop training programs to promote innovation, development, and deployment of new evidence-based solutions.
Impact Assessment
To ensure that the global digital health system for NCDs, once developed, is generating expected outcomes, the establishment of a regular impact assessment and feedback mechanism is necessary. This brief proposes the adoption of Health Impact Assessment (HIA) developed by the WHO. HIA is a comprehensive and effective approach used to identify the potential health benefits of a policy and/or programme on a population, especially vulnerable or disadvantaged groups. HIA’s systematic step-by-step approach that includes methods such as scoping, screening, appraisal, reporting, and monitoring can help the G20 gauge potential needs, impacts, and scalability insights for policy development.
Figure 5: Health Impact Assessment
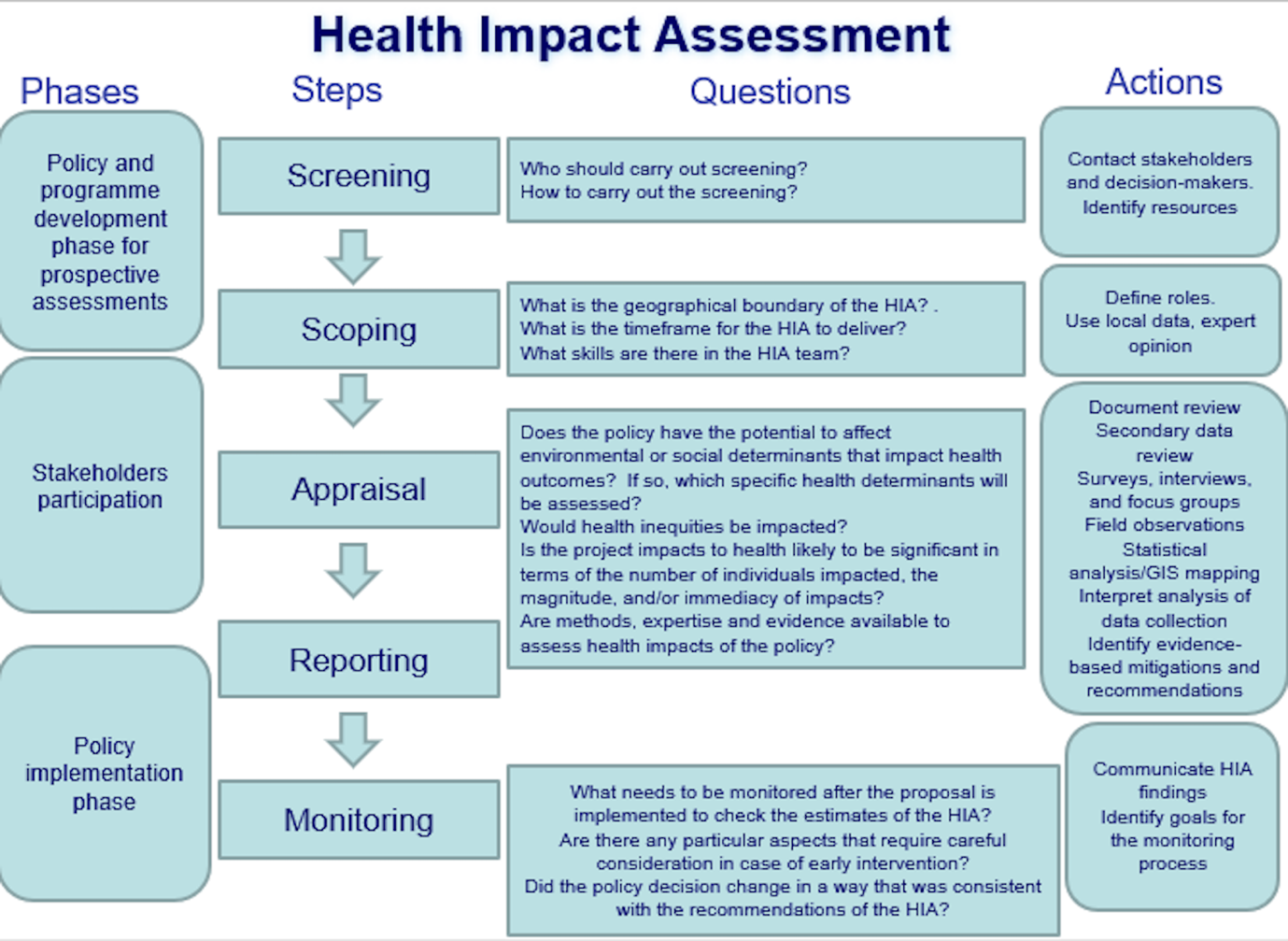
Source: WHO[17]
Attribution: Shipra Dawar and Sanjana Palakodeti, “A Global Digital Health System for Non-Communicable Diseases: Advancing Holistic Outcomes and Universal Health Coverage,” T20 Policy Brief, July 2023.
Endnotes
[1] “Noncommunicable Diseases,” World Health Organisation, September 16, 2022.
[2] WHO, “Noncommunicable Diseases”
[3] “Noncommunicable Diseases: Mortality,” World Health Organisation, accessed April 4, 2023.
[4] WHO, “Noncommunicable Diseases: Mortality”
[5] James E Bennet et al., “NCD Countdown 2030: Worldwide Trends in Non-Communicable Disease Mortality and Progress towards Sustainable Development Goal Target 3.4,” The Lancet 392, no. 10152 (September 2018): 1072–88.
[6] WHO, “Noncommunicable Diseases”
[7] WHO, “Noncommunicable Diseases: Mortality”
[8] “Global NCD Compact 2020-2030,” World Health Organisation, accessed April 4, 2023.
[9] WHO, “Global NCD Compact 2020-2030”
[10] Melanie Y Bertram et al., “Investing in Non-Communicable Diseases: An Estimation of the Return on Investment for Prevention and Treatment Services,” The Lancet 391, no. 10134 (May 2018), 2071–78.
[11] Aida Budreviciute et al., “Management and Prevention Strategies for Non-Communicable Diseases (NCDs) and Their Risk Factors,” Frontiers in Public Health 8, no. 574111 (November 26, 2020).
[12] Bertram et al., “Investing in Non-Communicable Diseases,” 2071–78
[13] Shangzhi Xiong et al., “Digital Health Interventions for Non-Communicable Disease Management in Primary Health Care in Low-and Middle-Income Countries,” Npj Digital Medicine 6, no. 1 (February 2023), 12.
[14] Xiong, “Digital Health Interventions for Non-Communicable Disease Management,” 12.
[15] World Health Organization, Tackling NCDs: ‘best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases, WHO, 2017.
[16] Elizabeth Murray et al., “Web-Based Self-Management Support for People with Type 2 Diabetes (HeLP-Diabetes): Randomised Controlled Trial in English Primary Care,” BMJ Open 7, no. 9 (September 2017): e016009.
[17] “Health Impact Assessment,” World Health Organization, accessed April 4, 2023.





