Task Force 6: Accelerating SDGs: Exploring New Pathways to the 2030 Agenda
Abstract
More than half of the world’s malnutrition disease burden is borne by the G20 countries. This includes malnutrition related to undernutrition, obesity, and noncommunicable diseases. This policy brief recommends the G20 countries affirm a target of reducing the malnutrition burden by 50 percent by 2030. Further, it suggests the establishment of a permanent G20 Nutrition Institute to provide an array of nutrition related recommendations (which can include broad principles on tackling malnutrition, such as the separation of public vs. clinical nutrition interventions, the creation of a dedicated nutrition cadre, and the establishment of a nutrition ministry as part of national governance structures). It also recommends the G20 take the lead in shifting the focus on the impact of malnutrition away from deaths and incidences towards disability adjusted life years.
1. The Challenge
Malnutrition continues to be a huge concern for the health of the global population. The World Health Organization (WHO) defines malnutrition[1] as “deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients.” It categorises malnutrition into three broad groups of conditions, namely, undernutrition,[a] micronutrient-related malnutrition,[b] and obesity and diet-related malnutrition.[c]
The world, especially developing countries, are facing the dual burden of malnutrition. On the one hand, the majority of a country’s population suffers from undernutrition and on the other hand, a significant portion of the population suffers from overnutrition related diseases. For instance, according to the latest government data from India,[2] 18.7 percent women and 16.2 percent men in the age group of 15-49 years suffer from undernutrition (BMI <18.5 kg/m2). At the same time, 21 percent women and 24 percent men also suffer from overnutrition (BMI > 25.0kg/m2).
Malnutrition is a complex condition resulting from a range of factors, including inadequate dietary intake, poor food quality, insufficient access to healthcare, and underlying health conditions. It can have significant adverse effects on physical and cognitive development, immune function, and overall health.
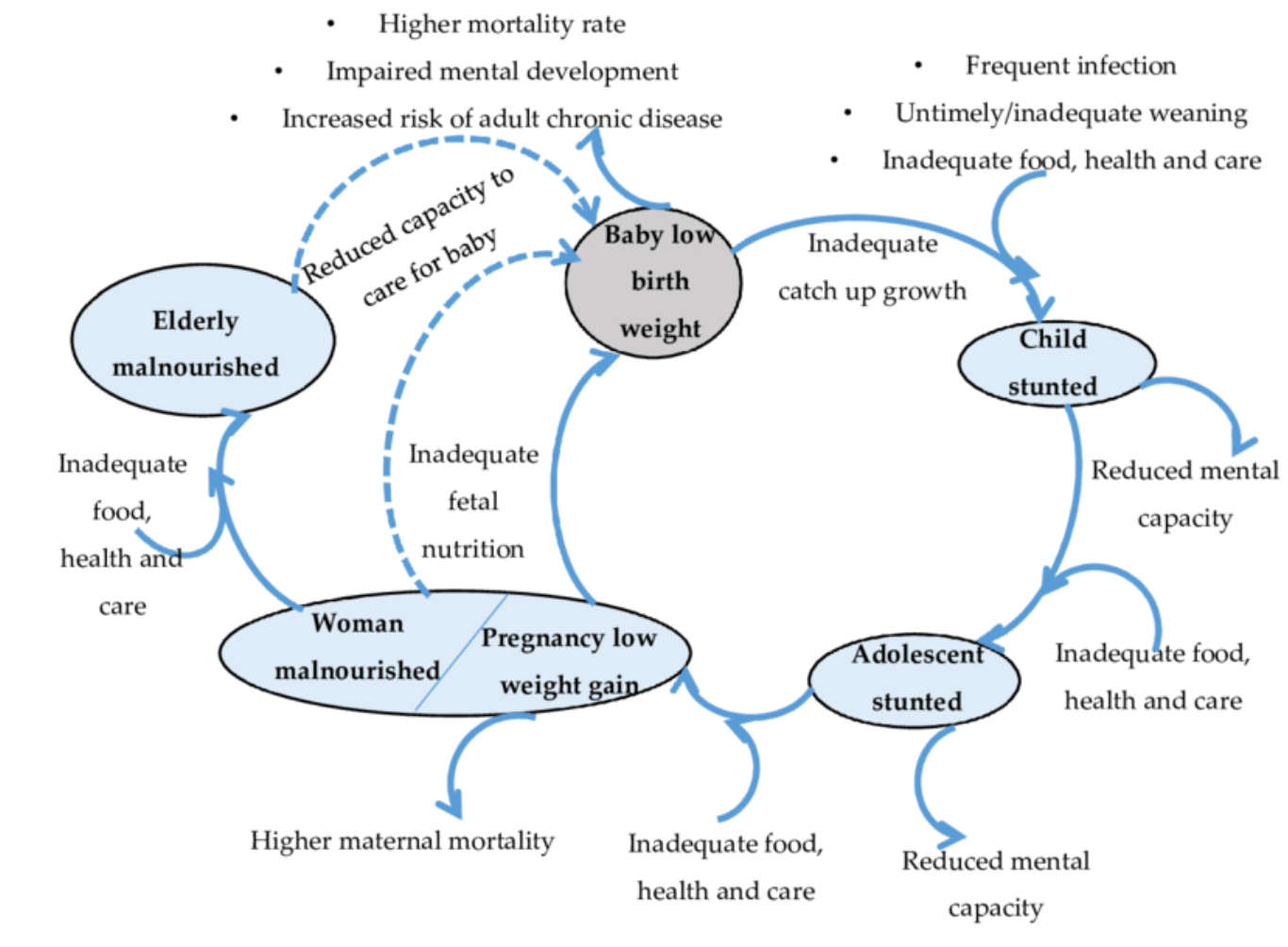
The lifecycle approach illustrates that undernutrition in children can result in long-term stunted growth, delayed cognitive development, and increased susceptibility to infectious diseases (see Figure 1).[3]
Figure 1: The life cycle approach to undernutrition
The first three years of life, also referred to as the “first 1000 days,” are crucial for a child’s cognitive development, and hence interventions during this period have the highest potential to reduce malnutrition and its impact. It is also demonstrated that if proper nutrition and care is not provided to children in these years, the damage may be irreversible.[6]Chronic undernutrition in adults can lead to wasting, muscle loss, and weakened immune function, as well as an increased risk of chronic diseases such as diabetes, cardiovascular disease, and certain cancers. Overnutrition can lead to obesity, metabolic disorders such as diabetes and hypertension, and an increased risk of cardiovascular disease, stroke, and certain cancers.[7]
One of the most significant effects of malnutrition on society is its impact on economic productivity. Malnourished individuals are more likely to experience poor physical and cognitive development, which can limit their ability to participate in the workforce and contribute to economic growth. In addition, malnutrition can lead to increased healthcare costs and reduced productivity due to illness and disability, which can have significant economic consequences for individuals, families, and communities.[8]
The G20 countries carry nearly 50 percent of this malnutrition burden (see Figure 2). Of the G20 countries, India has the largest proportion of disease burden (see Figure 3), making it the ideal candidate to champion for global solidarity to deal with this problem. Hence, tackling malnutrition should be a major concern for India’s G20 presidency.
Figure 2: The global distribution of malnutrition disease burden (calculated using disability adjusted life years)
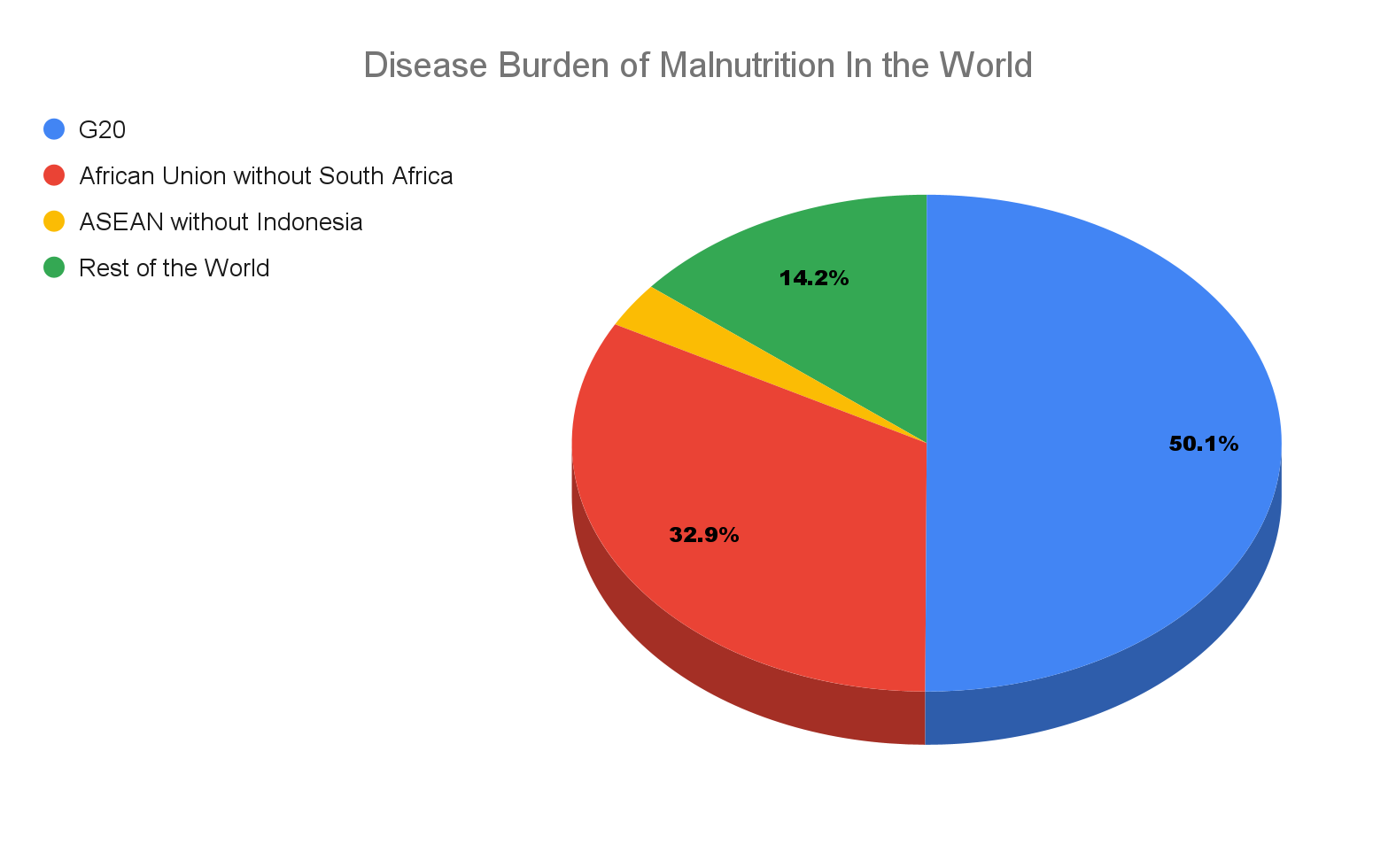
Source: Institute for Health Metrics and Evaluation, University of Washington[9]
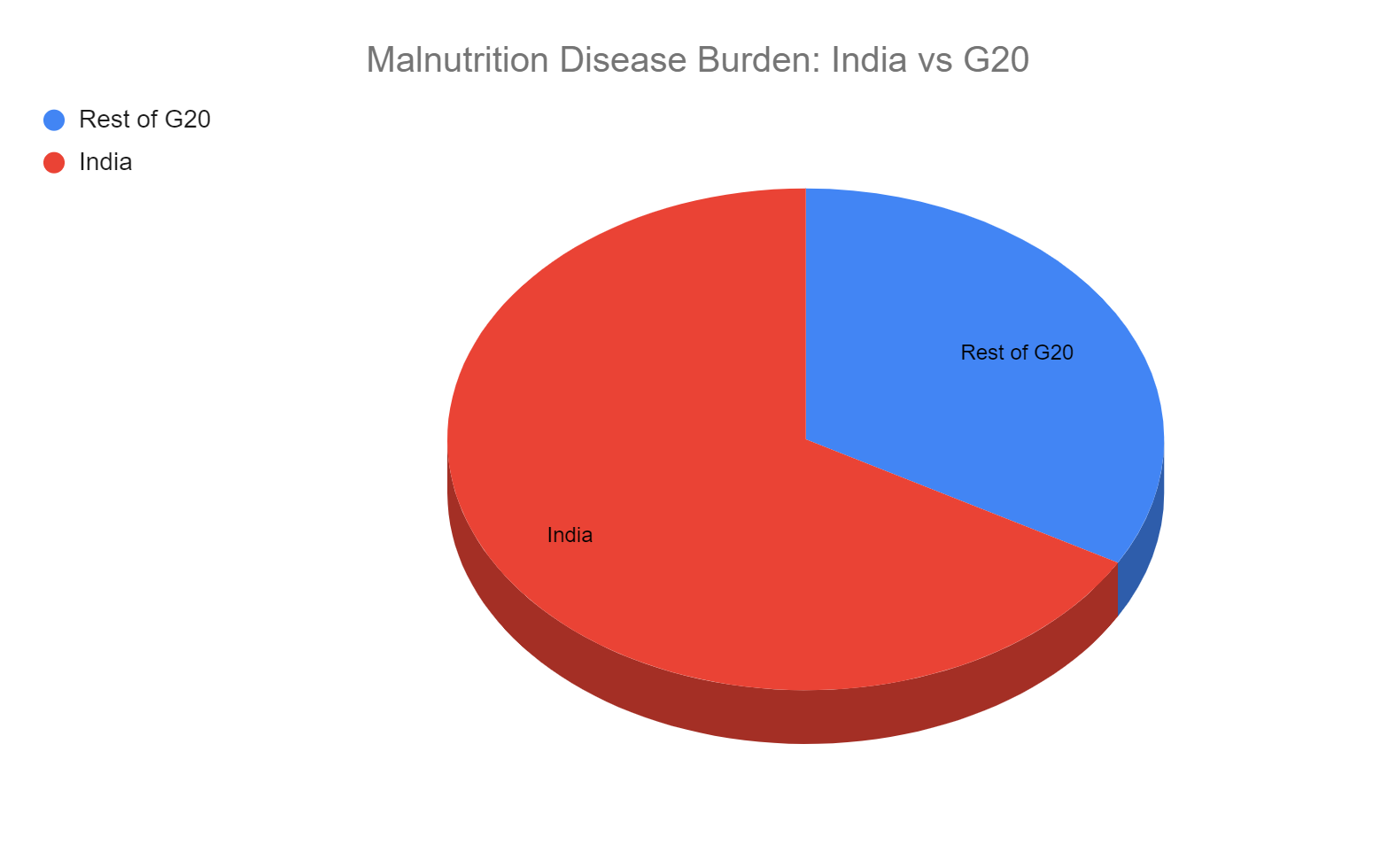
Source: Institute for Health Metrics and Evaluation, University of Washington[10]
Although malnutrition has improved around the world, the goal is not yet within reach. For instance, around the world, 22 percent of children still suffer from stunting and 6.7 percent from wasting. 5.7 percent of the world’s children are now overweight, and the number of children suffering from obesity has also increased.[12]
There is no one singular agency that is looking to alleviate malnutrition in the world. The United Nations Children’s Fund focuses on malnutrition in children and adolescents, and on maternal nutrition.[13] It works to ameliorate malnutrition related to undernutrition. The UN has also declared 2016-2025 as the Decade of Action on Nutrition.[14] This is a commitment to the sustained and coherent implementation of policies, programmes, and increased investments to eliminate malnutrition in all its forms. Still, there isa long way to go to achieve the goal of eliminating hunger and malnutrition entirely.
2. The G20s’s Role
The G20, as a group of the world’s largest and most influential economies, has a unique opportunity and responsibility to spearhead efforts to end malnutrition globally. Malnutrition is a major global health issue that affects millions of people, particularly in developing countries, and has far-reaching economic and social consequences. The G20, along with the African Union and Association of Southeast Asian Nations (ASEAN), carry the major share of the global malnutrition disease burden. The G20’s collective power and resources can help address this challenge and achieve significant progress towards ending malnutrition.
According to predictions, more than half of the countries in the world will not achieve the goal of eradicating hunger and related goals such as reduction in extreme poverty by the predetermined 2030 timeframe.[15] This means that without sustained effort and resource allocation, the world will not be able to alleviate the burden of hunger and malnutrition.
3. Recommendations to the G20
According to current estimates, the world is not on the path to achieving the desired reduction in malnutrition disease burden. Due to the COVID-19 pandemic, millions of children are yet again at risk of being stunted and wasted. Ending all malnutrition is not a goal that can be achieved by 2030, but with a push from G20, a 50-percent reduction in the malnutrition burden is achievable by 2030. This goal calls for evidence-based efforts that are driven by political will and include contingencies for sudden shocks such as pandemics. Our recommendations to the G20—of creating a G20 nutrition institute to drive efficient research and formulate policy interventions, and a nutrition cadre to operationalise these recommendations—will be key to achieving this goal.
-
Establish a permanent G20 nutrition institute
Overall, a G20-led policy institute that provides a list of policy interventions for countries to choose from can help to improve coordination, increase the impact of interventions, and ensure accountability in the use of resources. The G20 countries can pool their expertise and resources to create a more consistent and effective approach to policy interventions, leading to improved outcomes for populations around the world. The G20 have significant resources and expertise in a range of policy areas, and the establishment of a policy institute can be useful to create policy interventions that draw on best practices from a range of countries.
A G20-led policy institute can be potentially run in three ways:
- Independent organisation: The G20 countries can establish an independent organisation to run the policy institute. This organisation can have its own governance structure and staff, including researchers, policy analysts, and administrative personnel. The G20 would have complete control over the direction and priorities of the policy institute, as they would be the ones establishing and governing it. The organisation, running the policy institute would therefore be amenable to the needs and priorities of the G20. The creation of a new organisation will however be resource consuming and take considerable time to set up.
- Existing international organisation: The G20 countries could work with an existing international organisation, such as WHO or the UN to establish the policy institute. This could provide access to existing expertise and resources, as well as established governance and administrative structures. This option will be less resource intensive to set up. Working within the existing bureaucracy of an international organisation however can be challenging, and may slow down decision-making and implementation.
- Partnership with an academic institution: The G20 countries can partner with a leading academic institution, such as a university or research institute, to establish the policy institute. This can provide access to academic expertise and resources, as well as a network of researchers and policy experts.
In each of these scenarios, the G20 countries would need to determine the specific roles and responsibilities of the policy institute, including its focus areas, research priorities, and policy recommendations. The funding and resource requirements of the institute would depend upon the options. It would be easiest to operationalise this institute under WHO, with a portion of G20’s funding earmarked to WHO for this effort. This would allow the G20 to nucleate all activities around this problem, and use the inherent expertise and outreach of WHO to create and adopt recommendations related to malnutrition.
The proposed policy institute should focus on the following policy recommendations, which are based on globally applicable general principles for tackling malnutrition.
- Separation of public vs clinical nutrition interventions: Nutrition interventions can be broadly divided into two, the first being the public or community nutrition approach where nutrition is improved at the community level in response to a deficiency observed at that level. This approach is used to make improvements at a population level. A successful example of this approach in India is the addition of iodine to salt to prevent goitre and intellectual disabilities. This approach, which is mainly preventative in nature, includes educating people about dietary changes and helping them access optimum levels of nutrition. However, this approach is feasible only if the cause of malnutrition is common to the population. In 2021, Prime Minister Narendra Modi announced that fortified rice will be available under every government programme by 2024.[16] This scheme is an attempt to tackle anaemia caused by micronutrient deficiency. One of the major concerns with this approach is that the causes of anaemia affecting various segments of the population are different and may not be specifically caused by an iron deficiency. Therefore, supplying fortified rice at a population level will not solve this problem and instead could potentially lead to micronutrient excess in certain populations.[17]The second approach is clinical or personalised nutrition. In this, the focus is on the individual. This starts at a healthcare facility and includes modification of dietary factors of outpatient and hospitalised patients. Nutrition modification is also quite important in patients suffering from chronic diseases. Patients suffering from lifelong diseases such as diabetes, high blood pressure, and heart disease require constant support and guidance to be able to control them. Clinical nutrition plays an important role in that. The main aim of this approach is to prevent the progression and recurrence of diseases. We need to be able to choose which diseases require public nutrition interventions and which require clinical nutrition. The policy institute can help create frameworks to guide countries on how to better tackle problems of public versus clinical nutrition.
- Creation of a dedicated nutrition cadre: There are several reasons why countries should consider having a separate cadre of community health workers (CHWs) who are specifically focused on nutrition-related interventions. Existing CHWs, especially in developing countries, are overburdened[18]. A dedicated cadre of CHWs, who are trained and equipped to address nutrition-related issues can play a vital role in improving health outcomes and reducing the burden of malnutrition. They can provide targeted and effective support to individuals and communities who are most in need. These CHWs can receive specialised training in nutrition-related interventions and develop expertise in addressing specific nutrition-related challenges, such as malnutrition, anaemia, or stunting. These CHWs can work closely with local communities to identify and address specific nutrition-related challenges, such as micronutrient deficiencies or poor infant feeding practices. By focusing specifically on nutrition-related issues, these CHWs can provide more specialised and effective support than generalist CHWs who may have broader responsibilities.The CHWs can advise interventions across multiple sectors. They can work as nutritionists with medical doctors or help in creating school curriculum with a focus on nutrition or on recommending affordable nutritional options/substitutes for school lunch boxes. They can be attached to existing public primary healthcare infrastructure at the preferentially first rung of the healthcare system. They can also be integrated into the broader healthcare system to streamline resource allocation and prevent duplication. However, existing community healthcare workers should not be repurposed as nutrition healthcare workers. Instead, the nutrition cadre should be added to the existing workforce.
CHWs should be given the responsibility of non-nutrition related schemes such as immunisation and preschool education. Given that their training is deficient with regard to knowledge related to nutrition, training of CHWs should cover the causes of malnutrition, their effects, and the interventions, which can be used and moulded as per local conditions. The Philippines, a part of ASEAN, runs a cadre of Barangay Nutrition Scholars (BNS) who are responsible for providing nutrition education and support in their communities. BNS’ receive specialised training in nutrition education, growth monitoring, and food supplementation. A 2014 survey found that all respondents (mothers with children less than five years old) felt benefited from the programme and information imparted by the BNS.[19]
- More autonomy to local bodies to choose policies that suit their local conditions: Giving more autonomy to local governments to choose and implement nutrition interventions according to their needs and local conditions can have several benefits. It can promote the design of tailored interventions that are more effective in addressing malnutrition, engage communities in the development, and implementation of interventions, promote innovation and experimentation, and decentralise decision-making and resource allocation, thereby empowering communities to take greater ownership of their own health and well-being.
- Establish departments of nutrition at different levels of the government: Currently, different nations’ nutrition interventions are run by different departments, which include everything from health and family welfare departments to primary and secondary education departments. Due to the involvement of multiple departments of the government, coordination and cooperation becomes difficult. This also prevents the utilisation of the life cycle approach (previously mentioned in the document) to tackle malnutrition. Due to these two reasons, there is a need to overhaul and consolidate the government’s nutrition interventions into a single department (see Figure 4 for a structure of the proposed department).
Figure 4: Structure of proposed nutrition department
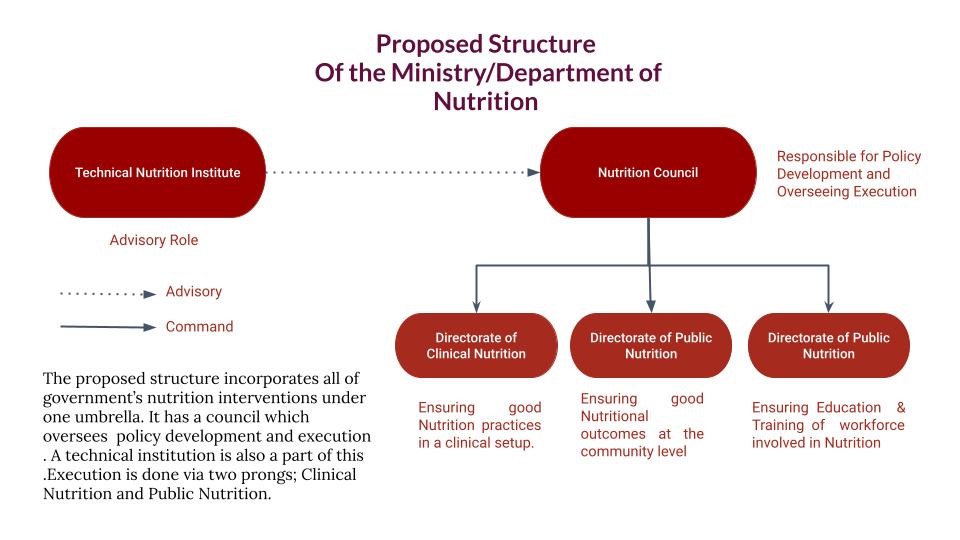
Source: Takshashila Institution[20]
- Better data collection and analysis: The use of impact indicators instead of uptake indicators[g] can have several advantages when it comes to measuring the effectiveness of nutrition interventions. Impact indicators measure the changes in nutrition status or health outcomes that result from the intervention, while uptake indicators measure the extent to which the intervention has been implemented or utilised. Overall, the use of impact indicators provides a more accurate and comprehensive measure of the effectiveness of nutrition interventions. They provide decision-makers with the information they need to make informed decisions about resource allocation, encourage a focus on outcomes, and promote greater accountability for those responsible for the design and implementation of interventions.
- Shift the focus on the impact of malnutrition to disability adjusted life years
The G20’s shift of focus towards disability adjusted life years (DALYs) can encompass risks and challenges, and present opportunities to reduce socio-economic stress for the problem at hand. DALYs represent the combined impact of premature deaths or years of life lost, and years lived with disability, resulting in a measure of the years of healthy life lost. Unlike death rate, which only considers mortality, DALYs are advantageous as they encompass both mortality and morbidity caused by a disease. DALYs can further be used to compare diseases and their impact on human life. For instance, with DALYs, you can compare the impact of acute Urinary Tract Infections with chronic disorders such as diabetes. It is also quite an effective tool to measure the impacts of policy interventions.
Attribution: Harshit Kukreja and Shambhavi Naik, “Reducing Malnutrition Across G20 Countries by Half by 2030,” T20 Policy Brief, June 2023.
Endnotes
[a] Undernutrition includes wasting (low weight-for-height), stunting (low height-for-age), and underweight (low weight-for age)
[b] Micronutrient-related malnutrition includes micronutrient deficiencies, including a lack of important vitamins and minerals, or micronutrient excess.
[c] Overweight, obesity, and diet-related malnutrition relates to noncommunicable diseases such as heart disease, stroke, diabetes, and some forms of cancer.
[d] SDG-2 aims to end hunger, achieve food security and improved nutrition, and promote sustainable agriculture.
[e] SDG Target 2.1 aims to achieve universal access to safe and nutritious food.
[f] SDG Target 2.2 aims to end all forms of malnutrition.
[g] Impact indicators assess the impact of an intervention, while uptake indicators only report on the intervention’s adoption. It is possible that a policy intervention may be popular, without necessarily having the impact that is desired.
[1] “Malnutrition,” World Health Organization, April 15, 2020, Accessed April 4, 2023.
[2] “Home | Ministry of Health and Family Welfare | Goi,” Ministry of Health and Family Welfare, Accessed April 4, 2023.
[3] Vinicius JB Martins et al., “Long-lasting effects of undernutrition,” International Journal of Environmental Research and Public Health 8, no. 6 (2011): 1817-1846.
[4] “4th Report − The World Nutrition Situation: Nutrition throughout the Life Cycle – UNSCN”, United Nations Administrative Committee on Coordination, April 2023.
[5] Ruth Shapu et al., “Knowledge, Attitude, and Practice of Adolescent Girls Towards Reducing Malnutrition in Maiduguri Metropolitan Council, Borno State, Nigeria: Cross-Sectional Study” Nutrients 12 (6), 1681 (2020).
[6] “Malnutrition in Children,” UNICEF DATA, Accessed April 4, 2023.
[7] Michael, Belay et al., “Overnutrition and Associated Factors Among High School Adolescents in Mid COVID-19 Pandemic in Ethiopia: Neglected Public Health Concern,” Adolescent Health, Medicine and Therapeutics (2022): 1-14.
[8] Karen Freijer et al., “The economic costs of disease related malnutrition,” Clinical Nutrition 32, no. 1 (2013): 136-141.
[9] “GBD Compare,” Institute for Health Metrics and Evaluation, University of Washington, Accessed April 4, 2023.
[10] “GBD Compare”
[11] “The 17 Goals | Sustainable Development,” United Nations, Accessed April 4, 2023.
[12] “Malnutrition in Children,” UNICEF DATA, Accessed April 4, 2023.
[13] “Nutrition,” UNICEF, Accessed April 5, 2023.
[14] “Decade of Action on Nutrition,” United Nations, Accessed April 5, 2023.
[15] Jonathan D. Moyer and Steve Hedden, “Are we on the right path to achieve the sustainable development goals?,” World Development 127 (2020): 104749.
[16] “Fortified Rice Available In Ration Shops In 439 Districts & Other Schemes: Govt,” Outlook, May 24, 2023.
[17] Sayantan Bera, “What’s Fortified Rice, Why Is Modi Govt Pushing it & Why Some Experts Aren’t Excited,” The Print, September 2, 2022.
[18] “ASHA Workers: The Underpaid, Overworked, and Often Forgotten Foot Soldiers of India,” Forbes India, June 26, 2021.
[19] El Ma Socorro, “Assessment of Barangay Nutrition Program implementation in selected municipalities in Ifugao, Bulacan and Siquijor: Community partners’ perspectives,” Acta Medica Philippina 48, no. 3(2014): 26-34.
[20] Harshit Kukreja and Shambhavi Naik, “Takshashila Discussion Slidedoc – a New Approach to Nutrition in Karnataka,” The Takshashila Institution, Accessed April 5, 2023.